Acinetobacter baumannii, a gram negative coccobacilli, is a major nosocomial infection involving the respiratory tract, bloodstream, skin and soft tissue, and the urinary tract.1 The SCOPE study by Wisplinghoff et al.,2 showed that A. baumannii was the second cause of death in patients admitted to intensive care units. In Thailand, in the report from the National Antimicrobial Resistance Surveillance Thailand Center (NARST), A. bauamannii was identified in the sputum during the year of 2017 as the second ranking pathogenic organism. In addition, this organism was ranked third of isolated clinical pathogens in Thailand.3 The increasing rate of A. baumannii worldwide might be from the multi-mechanisms of antimicrobial resistance and length of duration in a hospital environment.1
Due to increasing rates of infections and drug resistance, the antimicrobial choices for A. baumannii treatment are scant. Colistin, sulbactam, and tigecycline remain the last three options but the mortality rate and treatment failure remain varied.4 In Thailand, according to a previous study of antimicrobials used to treat multidrug resistant A. baumannii (MDR-AB) pneumonia at King Chulalongkorn Memorial Hospital, it was found that most patients receive a single sulbactam or sulbactam in combination with other drugs which accounted for 85.71 % of various regimens. Of in vitro colistin susceptibility, all A. baumannii were susceptible to colistin.5 The clinical experience of colistin use was evaluated at Siriraj Hospital, and it was found that 80.8 percent of patients with A. baumannii infection who received intravenously colistin had better clinical symptoms.6
Formally, the factors associated with death from A. baumannii infections were evident such as improper use of antimicrobial drugs, cancer patients, carbapenem-resistant A. baumannii (CRAB) infection, mechanical ventilation, toxic shock syndrome, septic shock, central venous catheter use, pneumonia, APACHE II score ≥ 14 points.7-9 However, the risk factor of mortality and treatment failure from various studies were uncertain and previous studies in Thailand usually included only CRAB infections, the overview of risk factors among all A. baumannii infections was absent. Moreover, such reports were often done in medical schools or large-sized hospitals. Thus, the severity of problems in a general hospital might be different to a private hospital. Therefore, the present study aimed to retrospectively collect data of patients infected with A. baumannii, to determine the treatment outcomes, risk factors associated with mortality and treatment failure. Our results might be useful to plan patient care to reduce unexpected outcomes in patients with A. baumannii infections.
This retrospective study gathered the data of patients infected with A. baumannii from January 2014 to December 2015, from the electronic medical records database. The protocol was approved by the institutional review board of Faculty of Pharmacy, Silpakorn University. This study was carried out to determine the treatment outcomes, risk factors associated with mortality and treatment failure of patients infected with A. baumannii.
Inclusion criteria:
Exclusion criteria:
Definitions
Combination antimicrobial therapy is a treatment with equal or more than 2 agents from different antibiotic classes. Appropriate antimicrobial therapy is a treatment with at least one active antimicrobial agent within 24 hours after reporting the result of susceptibility. Immunocompromised host included systemic lupus erythematosus, human immunodeficiency virus (HIV) infection, cancer, neutropenic patients (absolute neutrophil count <0.5×109 cells/L), patients with organ transplantation or immunosuppressive agents use (steroids at a dosage ≥ 10 mg of prednisolone daily for ≥ 2 weeks). Treatment failure included failure and death. Failure patients were ones whose clinical symptoms got worse or antimicrobial therapy had to be changed or added to against A. baumannii. Death was defined as deceased during hospitalization after A. baumannii infection.
Data Collection
Patient data were reviewed including age, sex, underlying diseases, ward, mechanical ventilator use, shock, hepatic function, renal function, immunocompromised status, antimicrobial regimens antimicrobial susceptibility based on disk diffusion method, length of hospitalization, source of infections, and clinical outcomes. The primary outcome measurements were all-cause mortality and risk factors related to failure and mortality.
Statistical Analysis
Descriptive statistics were used for in-hospital mortality and treatment failure rates of A. baumannii infections. Chi-square or Fisher’s exact test statistics analyzed the relationship between discrete factors and clinical outcomes. Mann Whitney-U test and t-test was used to compare the median and mean for continuous data analysis, respectively. The multivariate analysis by logistic regression was used. All statistical analysis was processed via R program, proposed α ≤ 0.05 as statistical significance.
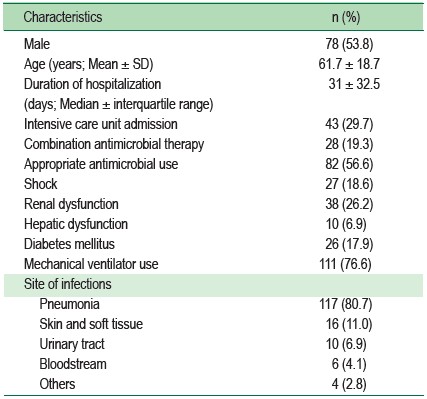
Of 298 participants with A. baumannii isolation, 145 participants according to inclusion criteria were included. Among them, 78 patients (53.8%) were male, mean age was 61.7 ± 18.7 years, median duration of hospitalization was 31 days, and 43 patients (29.7%) were admitted to the ICU. Pneumonia was the most common site of infection (80.7%) (Table 1).
Table 1: Characteristics of patients with Acinetobacter baumannii infections (n = 145)
Of the 145 A. baumannii cases, CRAB and MDR-AB accounted for 64.8% and 67.6%, respectively. Colistin monotherapy was used in 45 (31.0%) patients, carbapenem monotherapy was used in 36 (24.9%) patients, sulbactam monotherapy was used in 10 (6.9%) patients, colistin combination was used in 12 (8.3%) patients, and sulbactam combination was used in 7 (4.8%) patients.
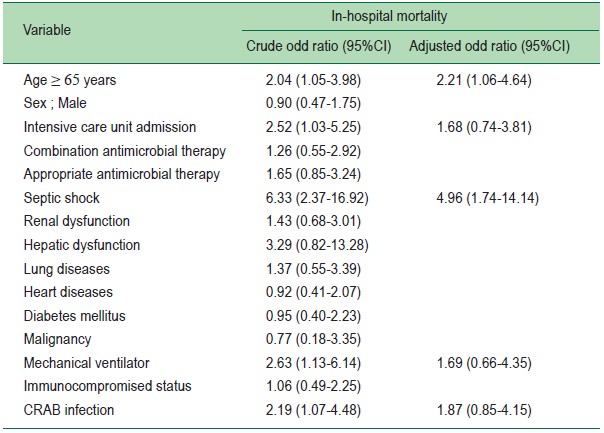
The in-hospital mortality and treatment failure rates were 43.4% and 52.4 %, respectively. The mortality rate was 42.4% for patients given monotherapy and 48.1% for patients given any combination therapy. The percentage of appropriate antimicrobial use was only 56.6%. For logistic regression analysis, shock was a statistically significant risk factor associated with treatment failure (adjusted odd ratios 3.10, 95%CI 1.21-7.97) and in-hospital mortality (aOR 4.96; 95%CI 1.74-14.14). Whereas age ≥ 65 years (aOR 2.21; 95% 1.06-4.64) was only associated with in-hospital mortality (Table 2).
Table 2: Univariate and multivariate analysis to identify risk factors influencing treatment failure among patients with Acinetobacter baumannii infections (n = 145) 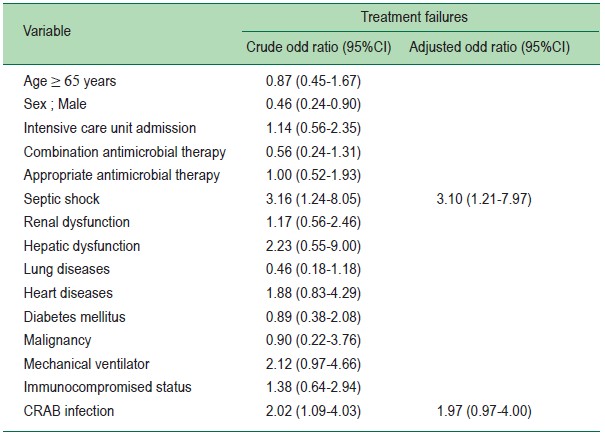
Table 3: Univariate and multivariate analysis to identify risk factors influencing death among patients with Acinetobacter baumannii infections (n = 145)
This present study indicated that the overall mortality rate for A. baumannii infections was 43.4% in a general hospital. However, our result seems to have a higher mortality rate than the previous two studies performed in Thailand, even those at university hospitals (33.8 and 30%, respectively).10, 11 We hypothesized that the results from different studies might vary in the mortality rate depending on patient status, age, underlying diseases, source of infection, and appropriate antimicrobial agents. Santimaleeworagun et al.,11 reported the overall mortality rate as 30% among cases with a higher percentage of appropriate antimicrobial use (82.7%) than in the present study (56.6%). Thus, the treatment outcome might be different, regardless of types of hospital.
This study showed that the presence of septic shock significantly increased the mortality rate and treatment failure among patients infected with A. baumannii. Our finding was similar to Kim et al.,8 and Inchai et al.,12 studies revealing shock related to 14-day mortality rate and 30-day mortality, respectively. As my previous study also found that septic shock significantly increased the mortality and treatment failure in patients infected with CRAB.9 Moreover, the present study indicated that age over 65 years which was associated with hospital death, being the same factor for in-hospital mortality in Brotfain et al., study.13
However, the appropriate antimicrobial treatment was not correlated with both mortality and treatment failure of patients infected with A. baumannii. The present results differed from our previous study9 and Inchai et al.,12 study indicating the proper antimicrobial use could reduce the mortality rate at 30 days and failed treatment with statistical significance. The explanation for insignificant analysis might result from the limitation of case’s data.
The septic shock and patients aged ≥ 65 years old were associated with unfavourable treatment outcomes in patients with A. baumannii infections. Thus, this critical condition has to be concerned to improve outcomes of A. baumannii treatment. According to the limitation of case’s data, a larger study could identify the risk factors for clinical outcomes based on the benefit of appropriate antibiotic therapy.
Thank you to the Microbiology Laboratory Unit of Hua Hin Hospital for bacterial strains data and to all authors for all aspects of the work.