Skin grafting is a simple surgical procedure for covering a wound. The skin graft survival process consists of three phases: plasma imbibition, inosculation, and revascularization. The major causes of partial or total graft loss are hematoma, seroma, and a shearing force; any one of these events interferes directly with the imbibition phase.Therefore, immobilization is an important procedure to secure the skin graft.
A number of securing methods have been reported. Some have been specifically designed for a high survival rate of skin grafts in various areas, such as bolster dressing, silicone rubber dressing,1 and hydrocolloid dressing.2 Negative pressure wound dressing (NPWD) was described by Morykwas et al. in 1997.3 A modified form of NPWD has been used for many kinds of wounds, including split-thickness skin graft (STSG) recipient sites. Foam-based NPWD has proved to be efficient and to significantly reduce the rate of STSG loss,4,5 and a 95% graft survival rate has been demonstrated by previous studies.6,7 Recently, gauze-based NPWD has been shown to be an alternative material for STSG immobilization, with a 96% survival rate for skin grafts.8 Gauzes are widely available and easy to apply. Moreover, they can be applied to complex, geometrical wounds, and wound exudation and bleeding can be reasonably assessed via the degree of gauze staining. We hypothesized that a gauze-based NPWT could be a useful alternative for the integration of STSG to the recipient wound site. We aimed to compare the STSG survival rates of gauze-based and foam-based NPWDs.
A comparative, prospective, single-blinded, cohort study was performed at the Division of Plastic Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University. The study was approved by the Institutional Review Board of Siriraj Hospital, Bangkok, Thailand (656/2560). All patients who underwent immediate wound coverage with STSG and NPWD placement for immobilization were included in the study. The NPWDs were removed on Day 7 in all cases. The techniques used for the gauze- and foam-based NPWDs were uncontrolled and depended on each surgeon’s preference. Patients under 18 years of age, with a history of abnormal bleeding, or with an allergy to the dressing materials, were excluded. Informed consent was obtained prior to participation in the study.
For the brief surgical technique, the STSGs were harvested by pneumatic dermatome and fenestrated with a No. 11 blade or a Brennen skin graft mesher. The grafts were then placed onto the recipient site and sutured to the wound bed using an Optime R absorbable suture (size 5.0; Péters Surgical, Bobigny, France) or metallic staples.
In the case of the foam-based NPWD group, each STSG was first covered with a single layer of paraffin gauze dressing (Bactigras, Smith & Nephew, Sydney, Australia), on top of which a sheet of polyurethane foam with a nasogastric tube no. 18 was then placed. Finally, an antimicrobial adhesive drape (3M Ioban 2 Antimicrobial Incise Drape; 3M Health Care, St. Paul, MN, USA) was applied over the whole system to create a closed spaced for negative pressure (Figure 1a). As to the gauze-based NPWD group, a gauze was used instead of polyurethane foam, as illustrated in Figure 1b. With both the foam- and gauze-based NPWDs, the nasogastric tube was connected to the wall-suctioned negative pressure system at minus 100 mmHg.
The NPWDs were removed on postoperative Day 7. The discharge from the tube was recorded daily. Pain scores were evaluated using a numeric rating scale before and after the removal of the dressing. Digital photographs, that used a flash, were taken of the wound with a ruler. Every 3 days, all patients had their wound dressings changed using lipido-colloid dressing materials (Urgotul SSD; Urgo Medical, Chenôve, France), and the patients were reevaluated on postoperative Day 30.
The areas of graft loss and success were evaluated by a blinded operator. Another operator calculated the size of each area using the ImageJ program (Figure 2). The success rates of the graft survival at postoperative Days 7 and 30 were assessed. The authors defined success as when the graft survival area represented more than 95% of the recipient area.
A t-test and Wilcoxon rank sum test were used to analyze continuous variables for simple comparisons, and the Krus- kal–Wallis test was used for multiple comparisons. All patients were analyzed in the group to which they were assigned, thereby adhering to the intention-to-treat principle. The con- tinuous variables are described as median and range, whereas the categorical variables are presented as a percentage unless indicated otherwise. A two-tailed alpha level of 5% was con- sidered statistically significant. All the confidence intervals are expressed at 95%. Moreover, a non-inferiority test with a non-inferiority margin of 0.1 was used to evaluate the non- inferiority of the success rate of the 2 groups on postoperative Day 30. The lower bound of the 95% one-sided confidence interval for the difference in the favorable outcomes of the foam-based and gauze-based NPWDs was greater than the pre-specified non-inferiority margin of -10%. PASW Statistics for Windows (version 18.0; (SPSS Inc., Chicago, IL, USA) was used for the data analyses.
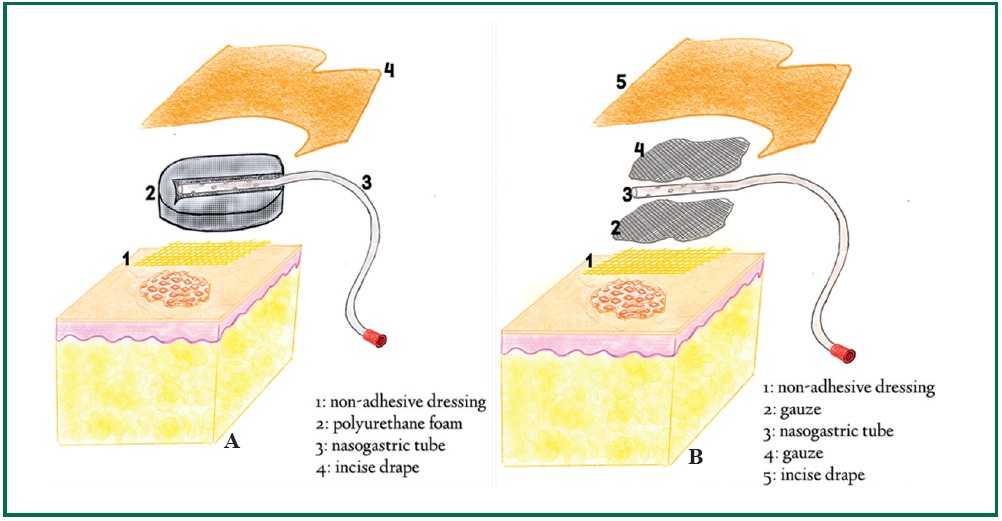
Figure 1: Diagram illustrating the technique for STSG immobilization; (A) shows the foam-based NPWD method, and (B) shows a gauze-based NPWD.
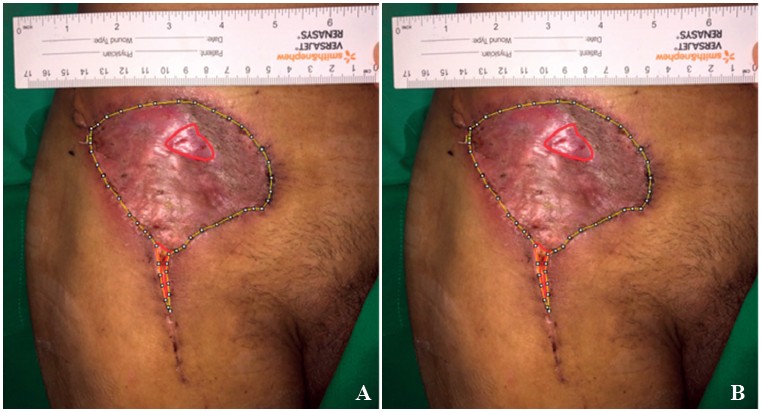
Figure 2: Evaluation of (A), the total area of a graft – dot lines, and (B), graft-loss – red lines, using the ImageJ program.
The study was carried out from October 2017 to February 2019. In all, 69 patients with 79 grafted wounds were in- cluded. The indications for skin grafting included immediate or delay wound coverage after tumor removal, delay coverage after infected tissue debridement and secondary defect cover- age after free flap procedures. Forty-two wounds were dressed with a foam-based NPWD, while 37 wounds had a gauze-based NPWD applied. By postoperative Day 30, 12 patients with 14 wounds had become lost to follow-up. The median ages of the foam- and gauze-based groups were 55.5 and 59 years, respectively (p = 0.233). Diabetes mellitus and dyslipidemia were found among the patients in the gauze-based group more often than among those in the foam-based group, with p of 0.082 and 0.039, respectively. However, patients with underlying hypertension and chronic kidney disease showed no significant
differences between the 2 groups. The data are detailed at Table 1.
No statistically significant differences in the graft survival rates of the 2 groups were found at Days 7 and 30, with 89.74% and 95.01% for the foam-based group, and 87.63% and 92.52% for the gauze-based group (p = 0.473 and 0.843), respectively (Table 2).
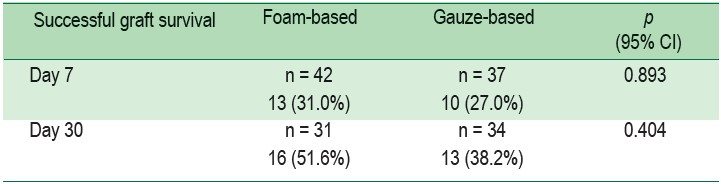
In this study we defined success as when the percentage of graft survival exceeded 95%. No statistical difference in the success rate was found in each group, with p = 0.893 for the foam-based group and p = 0.404 for the gauze-based group (Tables 3). The non-inferiority test using a z-statistic showed a p = 0.08841583, and the 95% one-sided confidence interval for the difference in the success rates of the 2 groups was -0.17279 to 1.00000.
Table 1: Demographic data of the patients in the foam- and gauze-based NPWD groups 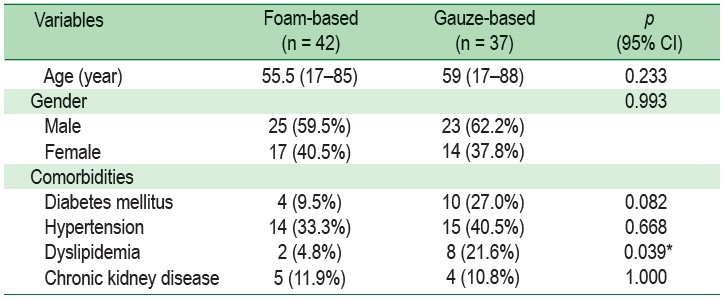
Table 2: Comparison of the area of graft survival of the 2 groups.
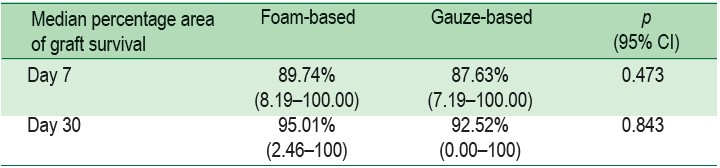
Table 3: Number of patients with an area of graft survival exceeding 95% at Day 7
STSG is a common and versatile procedure for wound coverage. The common causes of graft loss are fluid collection beneath the grafts and a shearing force. The technique of immobilization facilitates the neovascularization process and is therefore important for skin graft survival. The bolus and tie-over dressing techniques have been widely used as immobilization techniques. Recently, Vidrine et al.9 reported STSG healing was improved in an NPWD group (92%) compared with cases using bolus dressing and splinting (81%) at 4 weeks (p = 0.10). NPWD can improve the survival rate of STSG due to the immobilization of the graft (which improves the adherence of the graft to the wound bed) and the sucking out of the fluid (blood or seroma) that collects between the graft and the wound bed. A systematic review suggested that the use of foam-based NPWD for STSG was superior to traditional dressings in terms of the quality and quantity of survival. The authors of that review recommended the use of foam-based NPWDs for STSG, especially in the case of large, complex, exuding, and irregularly contoured wounds.7
Recent studies have demonstrated that gauze-based NPWD is safe and effective for STSG recipients.8,10,11 From our study, the median area of graft survival at postoperative Days 7 and 30 revealed no statistical difference between the 2 groups. There was a change in the surgical technique for the gauzed-based group: during the initial phase of the study, small pieces of damp gauze were placed over the STSG before placing the nasogastric tube. We observed that the graft survival was significantly low in the early stage of this study, with some patients having total STSG loss. In order to improve contact with the wound surface, we suggested to the surgeons that they place sheets—rather than small pieces—of damp gauze on the STSG. The data after the surgeons gained experience with the modified technique revealed a better graft survival (data not shown). As we included all patients in the gauzed-based group for data analysis purposes, as per the intention-to-treat strategy, we can see a range from 0% to 100% (Table 2). For the gauze-based NPWD procedure, we recommend that instead of using a number of small pieces of gauze as the first layer, a single large sheet should be used to facilitate contact with the surface of the graft area.
Dyslipidemia was found significantly more often among the patients in the gauze-based NPWD group than in the oam-based group, whereas diabetes mellitus was found more frequently in the gauze-based group (but without statistical significance). This suggests that we can utilize gauzed-based NPWD as an STSG immobilization technique for patients with underlying medical issues. The non-inferiority test showed that the gauze-based NPWD was non-inferior to the traditional foam-based NPWD for the STSG procedure. Nevertheless, the data also showed no statistical differences, which implies that the small sample sizes might have altered the outcomes. The difference in the demography of the population in this study was another limiting factor. A further randomized, controlled study should be performed.
In some circumstances, polyurethane foam is not available, resulting in the use of alternative material as the base for an NPWD. In contrast, gauze is available at nearly every medical center. A gauze-based NPWD should be the optimum choice for several reasons: it is versatile (being able to be applied to complex, geometrical wounds), is painless when removed, and facilitates the detection of complications detection.12–15 At our service, gauze-based NPWD costs around 500 Baht for each patient, whereas each foam-based NPWD costs over 2,000 Baht.
Our study indicates that the outcomes of using gauze-based NPWD for STSG immobilization are comparable with those of foam-based NPWD. The use of a gauze-based NPWD can be regarded as an alternative dressing technique for STSG after a surgical procedure.
The authors gratefully acknowledge Dr. Sasima Tongsai of the Division of Epidemiology, Faculty of Medicine Siriraj Hospital, for her professional statistical analysis. They also thank all attending staff at the Division of Plastic Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, for their support during the performance of this study.
The authors have no conflicts of interest or any funding to declare.