Lung cancer recurrence and metastasis from other organs is nowfrequently observed.1 For early stages, surgery remains the first choice oftreatment but recent studies reported that 2-5% of non-small cell lungcancer (NSCLC) patients later develop metastasis or tumor recurrence.2,3Late stage patients are not the best candidates for curative surgery due toextent of the disease, comorbidities and poor cardio-respiratory function.
PIMT is a rare benign tumor that constitutes 0.7% of all lung lesions.4-9Diagnosis through biopsy and radiologic exam is difficult due to its varyingcell characteristic and images. Management of this rare disease is dependenton the type of tumor, extent of disease and general health status of the patient.10For treatment purposes and to prevent recurrences, complete resection isnecessary. However, not all are valid candidates undergo surgery.11
There are other available treatment options both for early and latestages of lung cancer and inflammatory myofibroblastic tumor (IMT) thatare minimally invasive. These include chemotherapy, target therapy, radiotherapy and thermal ablation which are proven safe and effective managementoptions.1,12-15
MWA therapy is a technology that is image-guided and uses highfrequency microwave energy waves that produce tissue-heating effects todestruct solid tumors. It is less invasive, proven effective, preserves normallung parenchyma and can enhance the efficacy of chemotherapy and/orexternal beam radiation.16
The purpose of this study is to evaluate the safety and efficacy of MWAas an alternative treatment of lung tumors in different case scenarios.
In October 2016, a 69-year-old female patient came for a routinecheck-up. She was asymptomatic, non-smoker and had no family history oftuberculosis or lung cancer. Her chest x-ray showed an ill-defined noduleat left upper lung, measuring about 4.0x4.2 cm, with diffuse nodularopacity in both lungs. Computed tomography (CT) of chest revealedmultiple small nodules measuring 4 mm, 5 mm, and 6 mm at the right lower lobe, right middle lobe and right upper lobe, respectively.A 45x35 mm mass with ill-defined border was seen at the leftupper lobe (central to intermediate zone) together withmultiple small nodules of up to 5 mm in diameters. There werealso enlarged mediastinal nodes involved. EndobronchialUltrasound Guide Sheath (GS), Transbronchial Needle Aspiration(TBNA) and Electromagnetic Navigation Bronchoscopy (ENB)were performed and results revealed adenocarcinoma. Theepidermal growth factor receptor (EGFR), exon 19 deletionmutation was reported from her lung tissue specimen. Positronemission tomography (PET)/CT scan showed increased uptakefoci at the following sites: lymph nodes at left cervical(maximum standard uptake value (SUVmax) 5.16), rightlower cervical-supraclavicular (SUV max up to 7.02), and rightaxilla to subpectoral regions (SUVmax up to 4.93 at subpectoralnode). Left upper lobe mass SUVmax was 18.33. A diagnosisof lung cancer (adenocarcinoma) stage IV was made andGefitinib 250 mg, 1 tablet once daily, was prescribed.
A month after the first dose of treatment, plasma EGFRbecame negative of mutation. Four months thereafter, a followupPET/CT scan revealed marked regression and moderatesize reduction of the primary malignant tumor. The tyrosinekinase inhibitor (TKI) was continuously provided for a yearuntil her follow-up chest CT scan in November 2017 showedthat those multiple small metastatic nodules were stable-toslightlyincreased in size. The primary lesion at left upper lobeCase # 2This is a case of a 29-year-old male from the Middle East,diagnosed with IMT. In December 2016, he was admitted toa local hospital in his country due to fever and cough. Initialdiagnosis was multilobar pneumonia and this was managedby antibiotics but he was unresponsive. Chest CT scanreported multifocal pneumonia complicated by left lower lungabscess, few mass-like opacities seen in the right lung withenlarged lymph nodes. Differential diagnosis was lymphomaversus bronchoalveolar carcinoma. Bronchoscopy wasperformed and revealed narrowed posterior segment of rightupper lobe. Mucosa of upper lobe is found to be erythematousand swollen. Pathology was negative of aspergillus antigen,malignancy or pneumocystis pneumonia. Additional tests werealso negative of HIV, pneumococcal, mycoplasma,chlamydia serology and mycobacterium infections. CTguided biopsy was done and revealed segmental interstitialfibrosis with chronic inflammation composed of lymphoid cellsand few eosinophil with no evidence for malignancy, TB orlymphoma. At this time, he was prescribed with low dosecorticosteroids and Azathioprine.itself had also increased in size from 2.7x1.8 cm to 3.2x2.0cm and a new daughter nodule was found at the posteriorborder of the primary lesion. Repeat plasma EGFR remainednegative, CEA was 4.66 ng/mL, and EGFR from repeat tissuebiopsy was negative of mutation and resistance. Cytology fromrepeat EBUS was positive for adenocarcinoma. She refusedto undergo chemo- and radiation therapy and preferred onlysurgical management. However, the cardiovascular surgeonadvised that surgery was not an option owing to her poorgeneral health and the metastases of the disease. Later, shedeveloped moderate hemoptysis. MWA as palliative therapywas offered as an option.
Ablation planning using her chest CT scan result, toconfirm the size and location, was done. Lesion sizes weremarked from coronal plane diameter (2.60 cm) and sagittal planediameter (3.18 cm). Under intravenous sedation, grid andneedle guide were applied to the marked lesion. Emprintpercutaneous antenna was inserted into the target tumorthoroughly. A CT scan was then preformed again to confirm theright location. Once the correct position was established,Emprint MWA at 100 watts was applied for 4 minutes to coverall areas of the tumor. No complication (such as pneumothorax,pleural effusion or bleeding) was observed. Immediatelypost-MWA, no more hemoptysis was noted. She was advisedto take TKI treatment. Eight months post MWA, PET/CT scanreported progression of intra-pulmonary metastasis.
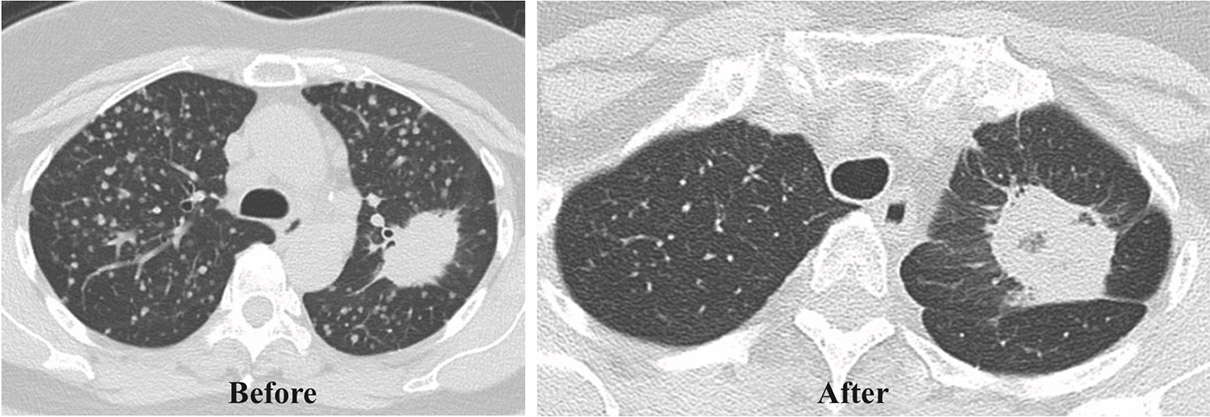
Before MWA shows the left lung mass. A month after MWA shows the continuous burning effectfrom MWA to the lung mass.
Figure 1: Chest CT scan of Case# 1
This is a case of a 29-year-old male from the Middle East,diagnosed with IMT. In December 2016, he was admitted toa local hospital in his country due to fever and cough. Initialdiagnosis was multilobar pneumonia and this was managedby antibiotics but he was unresponsive. Chest CT scanreported multifocal pneumonia complicated by left lower lungabscess, few mass-like opacities seen in the right lung withenlarged lymph nodes. Differential diagnosis was lymphomaversus bronchoalveolar carcinoma. Bronchoscopy wasperformed and revealed narrowed posterior segment of rightupper lobe. Mucosa of upper lobe is found to be erythematousand swollen. Pathology was negative of aspergillus antigen,malignancy or pneumocystis pneumonia. Additional tests werealso negative of HIV, pneumococcal, mycoplasma,chlamydia serology and mycobacterium infections. CTguided biopsy was done and revealed segmental interstitialfibrosis with chronic inflammation composed of lymphoid cellsand few eosinophil with no evidence for malignancy, TB orlymphoma. At this time, he was prescribed with low dosecorticosteroids and Azathioprine.
In June 2017, he was re-admitted due to hemoptysis. ChestCT scan showed interval reduction in the size of the right uppermass and mild reduction in the size of the left upper andlower lobe masses, interval increase in the number of smallbilateral nodular opacities. He was then screened for autoimmunedisease but had negative results. Bronchoscopy was repeatedand showed a clot in right upper lung bronchus. CT guidedbiopsy was performed and impression was organizingpneumonia versus IgG4 disease. He was managed byprednisolone 60 mg for 2 weeks, tapered gradually. The tissuespecimen slides were then sent to the United Kingdom (UK)for further studies. The opinion from the UK was IMT versuspneumonia versus IgG4 disease. ALK and ROSE studies werenegative. He was unresponsive to steroids and radiologicalappearance was not compatible with organizing pneumonia.Bronchial artery embolization and possible upper lobectomywere suggested but deferred due to patient’s condition.Hemoptysis was controlled conservatively and excisionalbiopsy was advised to obtain definite diagnosis. He thendecided to seek further management in Thailand.
In September 2017, mini thoracotomy and wedge resectionof the right upper lobe lung nodules were performed in adifferent medical facility in Thailand. Pathology reported IMT.The recommendation was targeted therapy treatment. He cameto our medical center for consultation and treatment options.Repeat Chest CT scan revealed consolidative mass like lesionat the right upper lung, measuring about 4.9x8.6 cm in size,with internal calcifications and mass extended in to the rightmain bronchus, multiple spiculate nodules at the both lungsare detected. A few of lymph nodes at the carinal region arealso noted. (Figure 2)
Physical examination revealed 15 kg body weight loss,mild dyspnea and occasional hemoptysis. Tumor debulkingusing rigid bronchoscopy was performed to destroy a part ofthe right upper lung mass obstructing the right main bronchus.Bleeding was controlled by argon plasma coagulation. Stent was placed on the right main bronchus to dilate the airway. Nocomplications were noted post procedure. MWA was advisedto treat unresectable lung tumors. The next day, MWA wasperformed on the remaining right lung mass. Lesion sizes wereright upper mass coronal plane diameter at 6.77cm andsagittal plane diameter at 8.28 cm. CT imaging was done toconfirm location. Under intravenous sedation, grid and needleguide were applied to the marked lesion. Normal saline bagof 1000cc was applied to avoid unnecessary burn. Emprintpercutaneous antenna is inserted into the right lung massthoroughly which was confirmed by chest CT scan. EmprintMWA 100 watts is applied for 10 minutes. Then, second locationwas navigated by CT scan. Antenna was pulled under thepleura and positioned to a different angle to reach the secondzone and lesion. Ablation 100 watts is applied for another 10minutes to cover all areas of the tumor. CT scan was repeatedto assess overall result and possible complications. No untowardsigns and symptoms were noted.
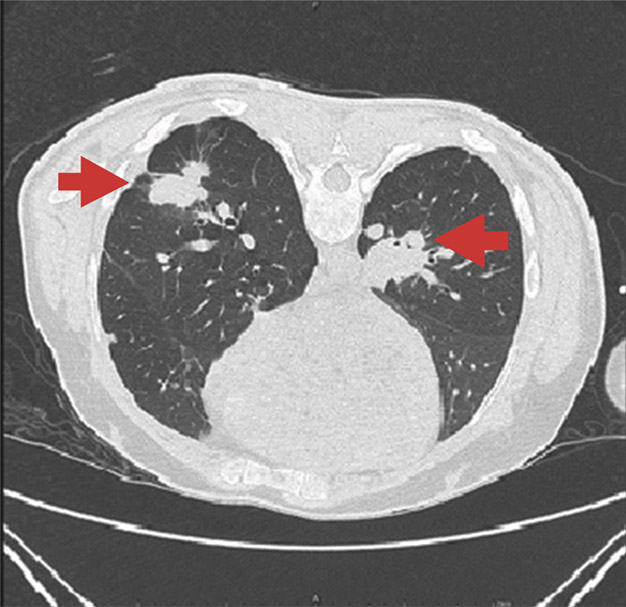
Figure 2.1: Chest CT scan image
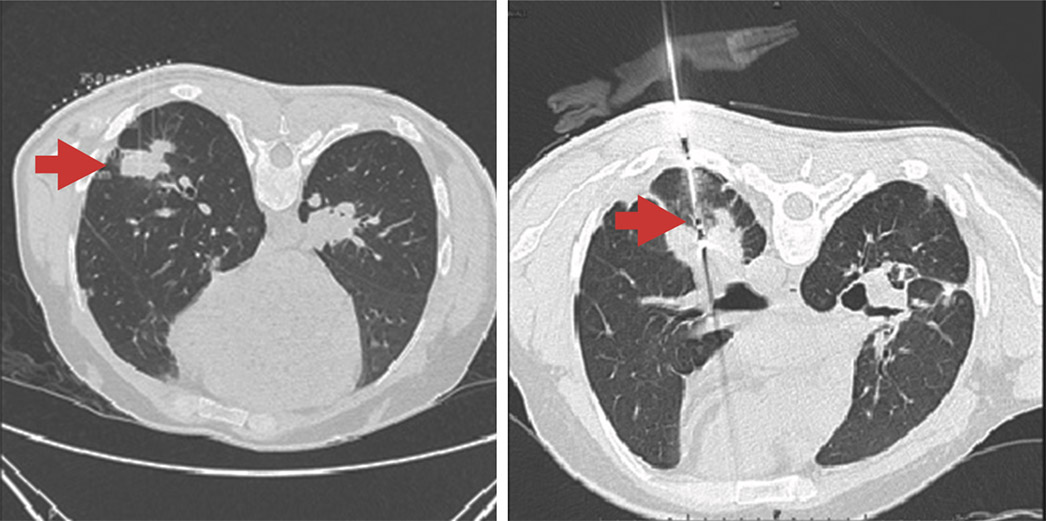
Figure 2.2: The first photo show the measurement and location of lesion prior to needle insertion ofMWA. Meanwhile, the second photo illustrates the needle inserted into the lesion.
A month following the first session of MWA, repeat chestCT scan reported continuous burning effect of MWA partiallydestructing the right upper lobe mass. A second session of MWAwas performed targeting the right lower lobe mass whichmeasures 2.60 cm coronal, 45 watts for 5.15 minutes was applied.Two weeks after the second session of MWA, the right upperlobe mass underwent repeat MWA which now measures 4.21cm coronal and 3.06 cm sagittal. The lesion is located at theright upper lobe which leaves a margin of 2.52 cm between theaorta and mass. CT image was done to confirm size and locationfollowed by application of grid and needle guide. Normal salineof 1000 ml was prepared to avoid unnecessary burns. Emprintpercutaneous antenna 20 cm was inserted and antenna penetratedthe center of the tumor. Overall shaft depth was 8.46 cm. ChestCT scan was again done to confirm proper position. EmprintMWA of 45watts in 4 minutes was applied. No untowardreactions were observed at the third session of MWA.
Six months after MWA, PET/CT scan reported metabolicprogression of existing mass at RUL, nodules at RLL and LUL.Unchanged hypermetabolic enhanced infiltrative intramusculartumor mass along the anteromedial aspect of the left proximalarm with cortical erosion of adjacent humerus.Case # 3This is a case of a 41-year-old female, foreign patient whocame for consultation due to difficulty with breathing andpersistent weight loss for a year. She was previously diagnosedwith pneumonia and was treated with antibiotics but wasunresponsive. She is a former smoker for 1.5 years. Chest CTscan reported right lung has infiltrative tumor involving entireright lung with size on axial plane = 12x8cm at right lower lobe,10.6 x 107cm at right upper lobe; tumor involving posteriorchest wall and right posterior ribs No. 7,8,9. There is inferiorinvasion of right diaphragm, serosal surface and parenchymaof right hepatic lobe. Visualized mediastinal lymph nodes were18mm in short dimension at right paratracheal region, 28mm atright tracheobronchial region, 39mm at subcarinal region. Thereis an 8mm nodule at superior segment of left lower lobe and12 mm cyst at left upper lobe. Tumor debulking using rigidbronchoscopy was recommended to extract part of the tumorblocking her airway. Stent placement was advised to help dilateair passage. Bleeding was controlled by argon plasmacoagulation. Cytology report was squamous cell carcinoma,PD-L1 (22C3) positive. PET scan reported intensely increaseduptake in infiltrative tumor in the right lung, more pronouncedin right lower lobe region with SUVmax up to 24.97. Invasionto diaphragm, adjacent ribs dome of liver is presented. Increaseduptake foci in mediastinal nodes are observed such as mattednode or mass and involved the subcarina and right hilum(SUVmax 15.79), right upper paratracheal (SUVmax 16.16)right lower paratracheal (SUVmax 13.83) and left lowerparaesophageal node SUV max 16.82. There is also increaseduptake in anterior diaphragmatic node (SUVmax 9.01).This is the first case of IMT reported to be destroyed byMWA. Also, this is the first known case of MWA used with stentplacement.
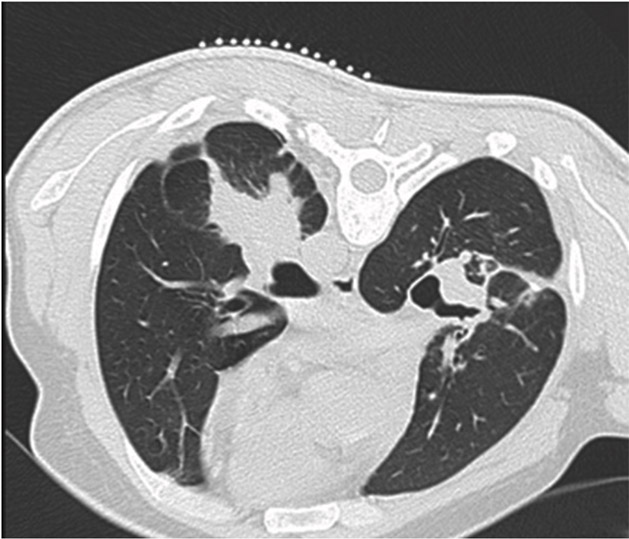
Figure 2.3: The burning effect of MWA a month after thefirst treatment session.
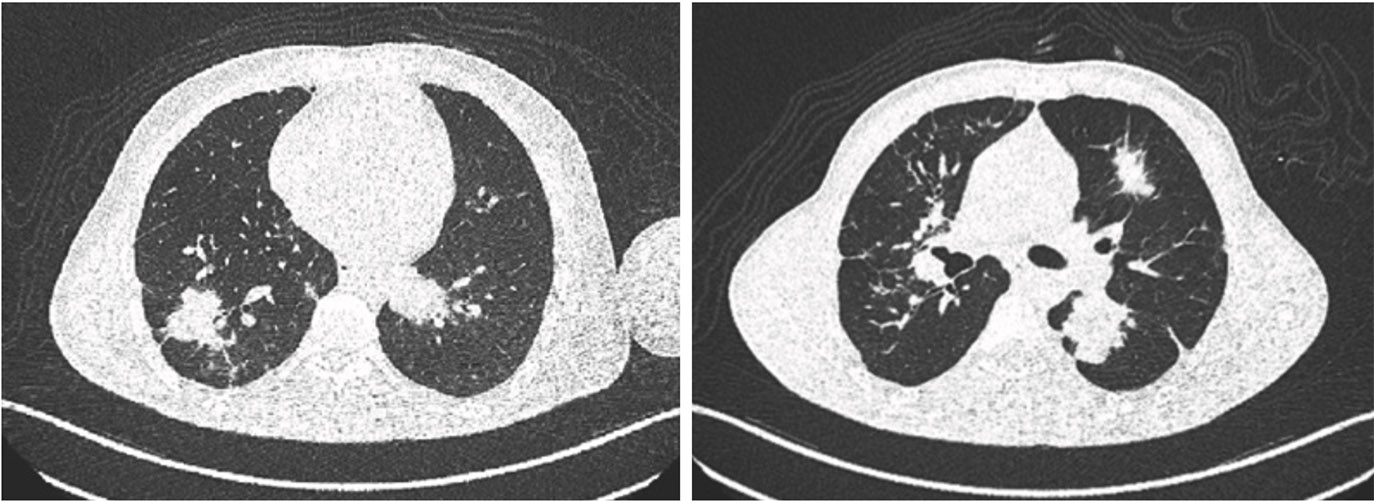
Figure 2.4: The CT scan images show the progression of lung mass.
This is a case of a 41-year-old female, foreign patient whocame for consultation due to difficulty with breathing andpersistent weight loss for a year. She was previously diagnosedwith pneumonia and was treated with antibiotics but wasunresponsive. She is a former smoker for 1.5 years. Chest CTscan reported right lung has infiltrative tumor involving entireright lung with size on axial plane = 12x8cm at right lower lobe,10.6 x 107cm at right upper lobe; tumor involving posteriorchest wall and right posterior ribs No. 7,8,9. There is inferiorinvasion of right diaphragm, serosal surface and parenchymaof right hepatic lobe. Visualized mediastinal lymph nodes were18mm in short dimension at right paratracheal region, 28mm atright tracheobronchial region, 39mm at subcarinal region. Thereis an 8mm nodule at superior segment of left lower lobe and12 mm cyst at left upper lobe. Tumor debulking using rigidbronchoscopy was recommended to extract part of the tumorblocking her airway. Stent placement was advised to help dilateair passage. Bleeding was controlled by argon plasmacoagulation. Cytology report was squamous cell carcinoma,PD-L1 (22C3) positive. PET scan reported intensely increaseduptake in infiltrative tumor in the right lung, more pronouncedin right lower lobe region with SUVmax up to 24.97. Invasionto diaphragm, adjacent ribs dome of liver is presented. Increaseduptake foci in mediastinal nodes are observed such as mattednode or mass and involved the subcarina and right hilum(SUVmax 15.79), right upper paratracheal (SUVmax 16.16)right lower paratracheal (SUVmax 13.83) and left lowerparaesophageal node SUV max 16.82. There is also increaseduptake in anterior diaphragmatic node (SUVmax 9.01).
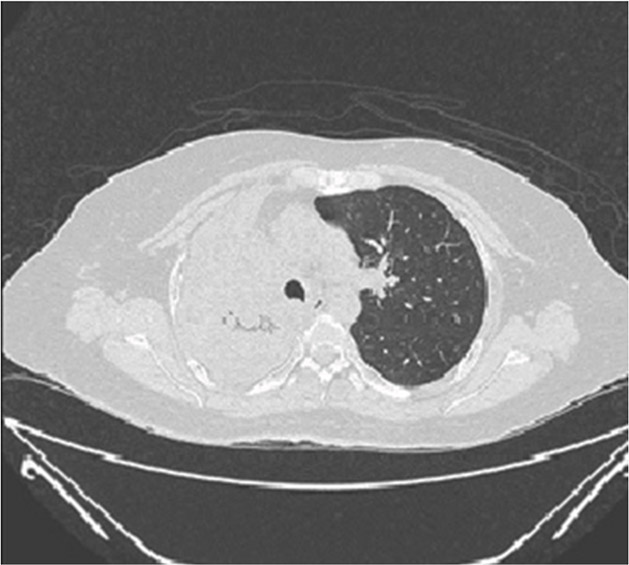
Figure 3.1: Chest CT scan shows the lung mass almost completely invading the right lung.
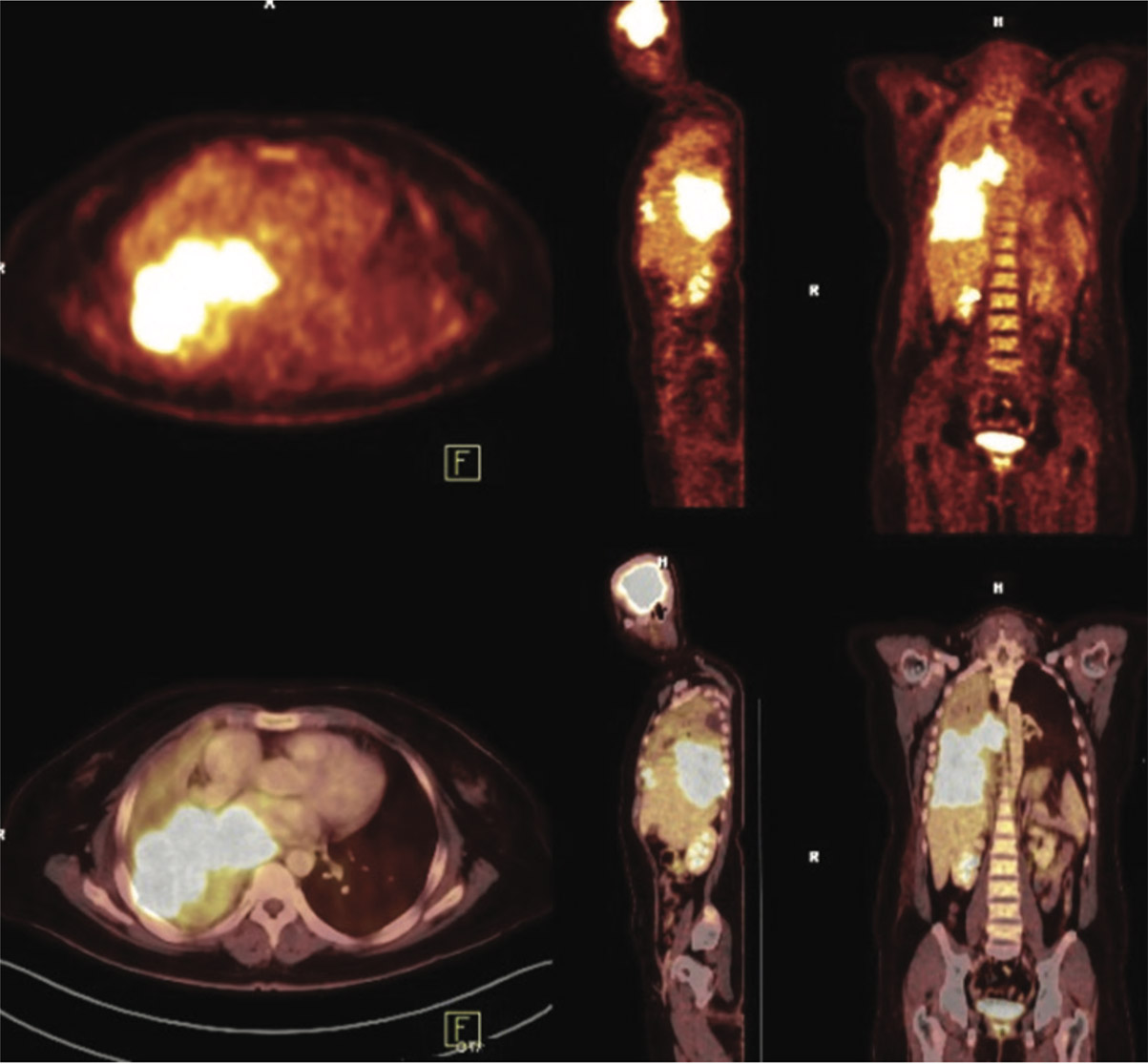
Figure 3.2: PET/CT scan exhibits increase uptake of right lung mass.
She was treated with 5 cycles of chemotherapy (Cisplatinand Gemzar) for 4 months. Post chemotherapy, follow up chestCT scan reported that there has been no obvious change in sizeof the rest of right lower lung mass, now showing as anirregular opacity with cavitary change at right lower lung,abutted adjacent pleura, encased proximal segmental and lobarbronchi, with rather decreased right pleural effusion andmildly increased aeration of right lower lobe. Her symptomsalso persisted. The Oncologist’s recommendation is for her toundergo another cycle of chemotherapy using a higher gradeof chemo drugs or immunotherapy but response to treatmentis unpredictable. She refused prolonged treatment and prefersto go to her home country. MWA therapy was advised tocompliment previous chemotherapy. She consented toundergo MWA. The target lesions were coronal planediameter 4.12cm and sagittal plane diameter 3.68 cm at rightlower lobe lung. Since the lesion is located near the diaphragm,the antenna was placed 2 cm above the diaphragm. CT scanwas done to confirm size and location. Under IV sedation, gridneedle was applied then emprint percutaneous antenna wasthoroughly inserted to the tumor. CT scan was again done tore-confirm position. Emprint MWA 45 watts for 2 minuteswere applied with predicted ablation zone of 1.8 cm diameterto ablate the tumor carefully. Chest CT scan was again doneto assess the result and possible complications. No immediateuntoward signs and symptoms were noted.
One month PET/CT scan follow-up reported almosttotal regression of the pre-existing large hypermetabolicmass in right lung with some residual pleural metastasis atright lung base. Total regression of the lymph node metastasesin right side of the mediastinum and paraesophageal node.No hypermetabolic lesion to suggest new metastasis.Healing of the locally invaded right posterior lower ribs.
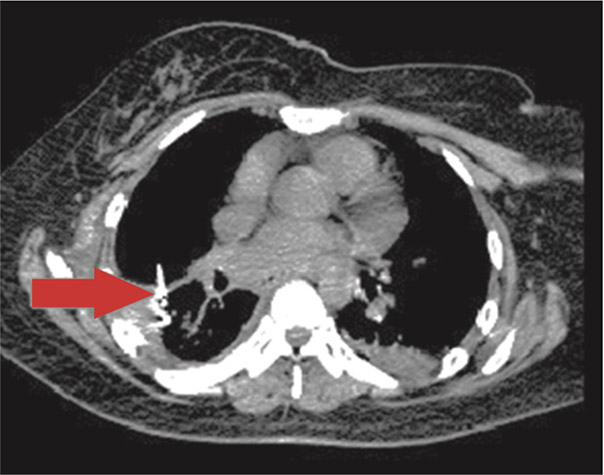
Figure 3.3: This illustrates the needle insertion into thelung mass prior to MWA being is delivered.
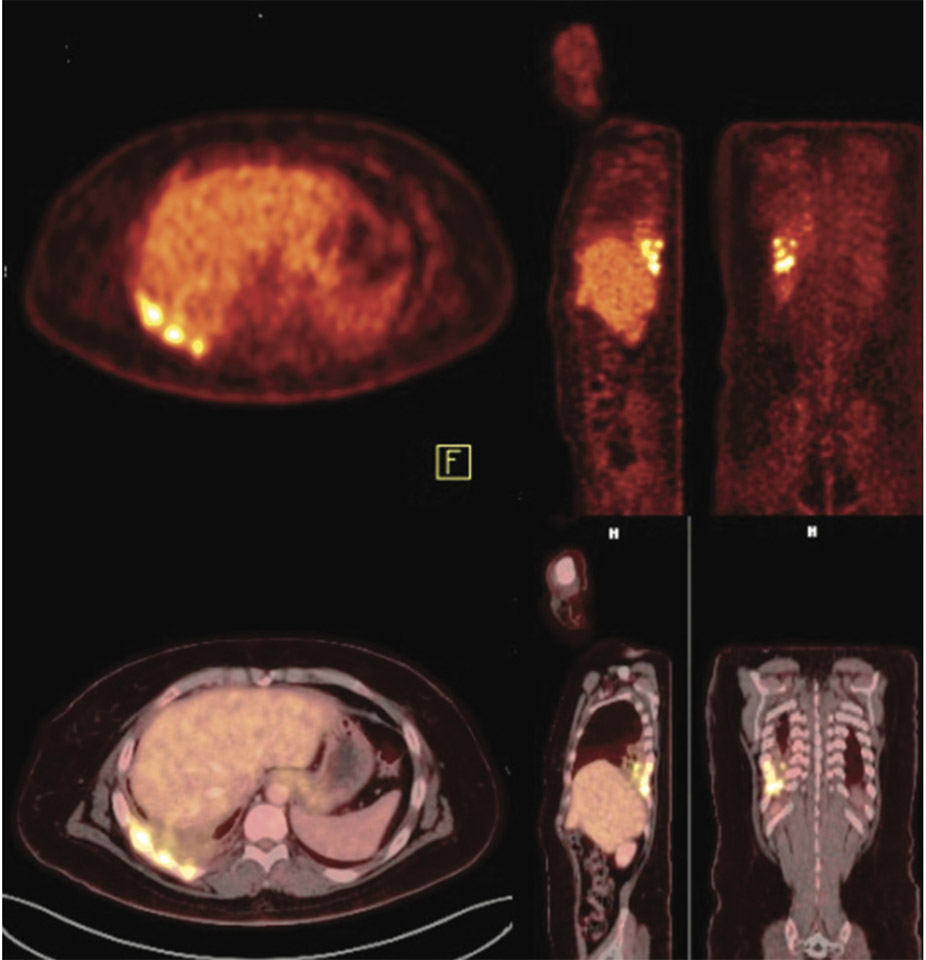
Figure 3.4: One month follow-up PET/CT scan after chemotherapy and MWAtherapy shows almost total regression of right lung mass.
This is a case of a 68-year-old female patient, diagnosedwith thyroid cancer, metastasis to the lung. In 2011, sheunderwent total thyroidectomy with radical dissection followedby modified right neck dissection and radioiodine I-131therapy in 2016. In 2017 she was diagnosed with malignantthyroid neoplasm: recurrent at right neck and had episodes ofmoderate hemoptysis and mild chest pain. Chest CT scanreported multiple various-sized nodules in both lungs, moreon the right lung, size up to 2.6 cm; the one at right hilumfocally obliterating right middle lobe bronchus and possiblyinvading anterior wall of adjacent right lower lobe bronchus.There is a 3.4x2.7x4.5 cm lobulated heterogeneouslyenhancing mass at right lower neck region, obliterating rightjugular vein and effacing right common carotid arteryanteromedially. Endobronchial Ultrasound TransbronchialNeedle Aspiration, Rigid bronchoscopy to debulk the tumorand stent placement to dilate the airway were performed.Pathology report was papillary neoplasm. The patient waslater lost on follow-up but came back after a year due torecurrent hemoptysis.
Chest CT scan revealed multiple enhancing pulmonary andsubpleural nodules scattering throughout both lungs, sized upto 2.6cm in diameter. The one at right hilum focally obliteratesright middle lobe bronchus and possibly invades anterior wallof adjacent right lower lobe bronchus. There is a5.0cmx4.1cmx3.6cm lobulated heterogeneously enhancingmass in right lower neck region, obliterating right jugular veinand effacing right common carotid artery anteromedially. Thereare two sclerotic lesions at T10 body and left 5th rib, size upto 0.9 cm. There is a suspected 1.8-cm hemangioma-like lesionat T6 body. Repeat tumor debulking and argon plasmacoagulation was performed to help clear her airway and stophemoptysis. The patient decided to be on palliative care andwas offered MWA therapy. The first lesion was located at rightlower lobe 1.76 cm near the diaphragm which measures 1.42cm, saggital. CT scan was performed to confirm the location.The percutanoues antenna was inserted 20 cm anteriorlythrough the tumor and overall shaft is 13.32 cm. MWA 45watts for a minute was applied. Predicted ablation zone is 1.4cm diameter. Repeat chest CT scan was done to check forcomplications.
Two weeks after the first session, MWA was performed atleft lower lobe lesion which measures 2.63 cm, coronal plane.CT scan was done to confirm location and size. Emprintpercutaneous antenna was inserted 15 cm from the lateral body.The antenna was pushed to the other side of the tumortouching the heart. The antenna is placed at the edge of tumorwhich leaves margin of over 2 cm from the heart. Overall shaftdepth was 8.24 cm. MWA 45 watts for 2.30 minutes wasapplied and predicted zone was 1.9 cm diameter. Air leak wasfound on post-procedure chest CT scan. This was managed byintercostal chest drain insertion. A day after, repeat chest x rayreported no more pneumothorax. No hemoptysis was observed.The patient did not come back for a follow up check-up.
MWA can be used to treat primary and secondarymalignancies. In this study, we reported how MWA is used tomanage four different cases of lung cancer and PIMT. The firstcase is diagnosed with adenocarcinoma then underwent TKItherapy but had tumor recurrence after a year of treatment.MWA is advised as palliative therapy. The second case isdiagnosed with IMT and received several treatments- evensurgery with no success. MWA is performed to shrink recurringtumors that obstructed his airway. The third case, diagnosedof squamous cell carcinoma received MWA to complimentchemotherapy. For the fourth case, thyroid cancer-metastasisto the lung, MWA is performed as palliative management andto help stop lung hemorrhage.
Surgical resection is the standard treatment with bestchance of disease remission and survival.16,17 However, in thisreport, all cases were poor surgical candidates. Minimalinvasive procedure such as MWA is the best option aspalliative care. The main objective of MWA for all of thesecases is to help maintain a patent airway by eradicating asmuch malignant cells while preventing further tissue damage.
There are several reports published that demonstratesMWA as an effective way to manage and control malignancies.In three studies, each with more than fifty subjects, yielded1-year survival rates reported 47.6% to 83%, 2-year survivalrates ranging from 23.8% to 73%, and 3-year survival ratesranging from 14.3% to 61%.16, 18-20 Our study, althoughreported only four cases, has further proven that MWA iseffective in different types of lung malignancies. All fourpatients tolerated the procedure well with one case ofpneumothorax.
MWA for four patients was administered under localanesthesia and moderate sedation. The MWA instrument thatwe used was Emprint Ablation System with ThermosphereTechnology. This system can produce 0 to 100 watts at2,450 + 50 MHz. A microwave antenna with gauge 14, 15 to20 cm length using circulation cooling system was placed intothe tumor with the guidance of chest CT scan. Once positionwas confirmed, ablation was performed with a power of 45 to100 watts for 1 to 8 minutes per site. The power and timedepends on the size of the target lesion as seen in Table 1below. Repeat chest CT scan was performed after MWA tocheck for air leak or other possible complications. Also, toprevent infection, antibiotic was administered prophylacticallybefore ablation.
Table 1: This table shows the amount of power and duration delivered to the lesion according to its size
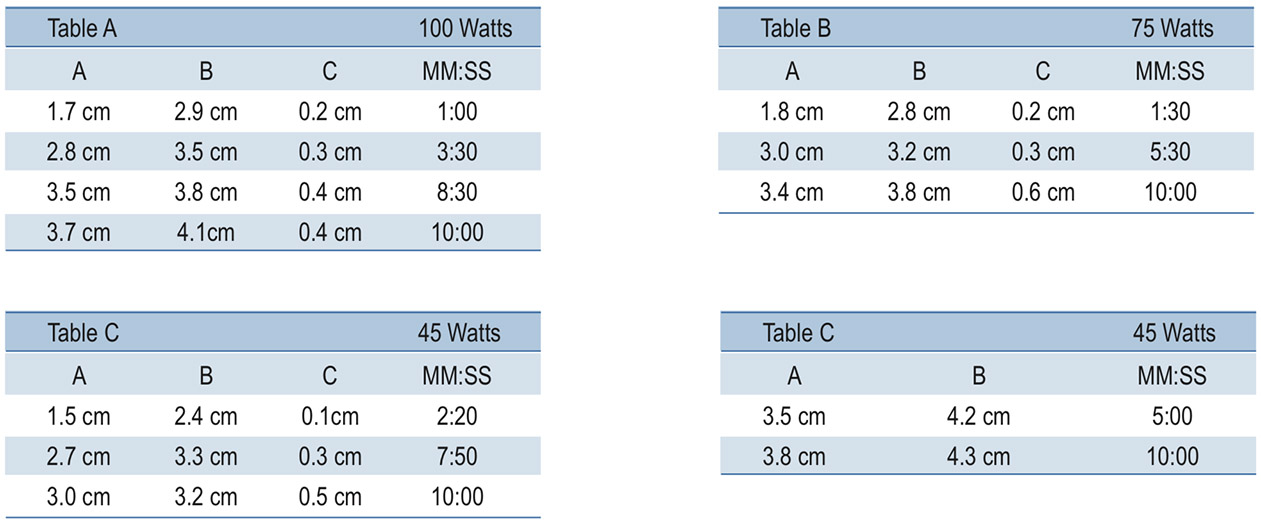
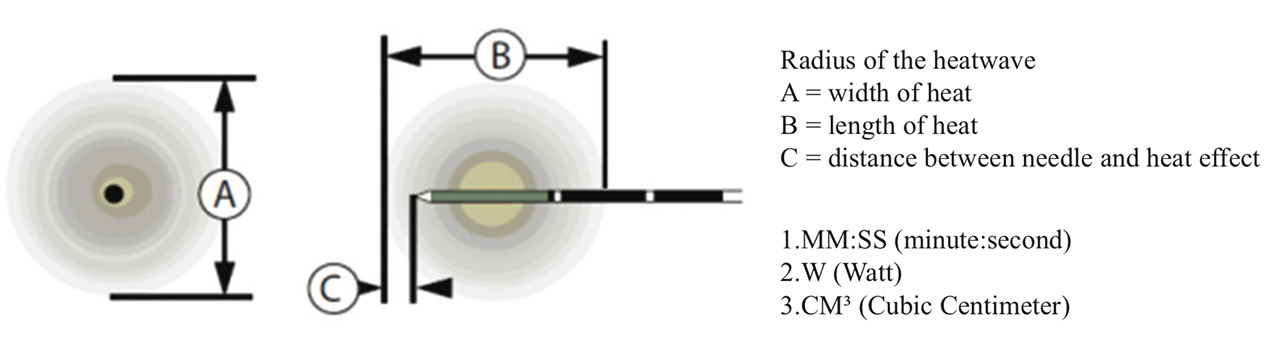
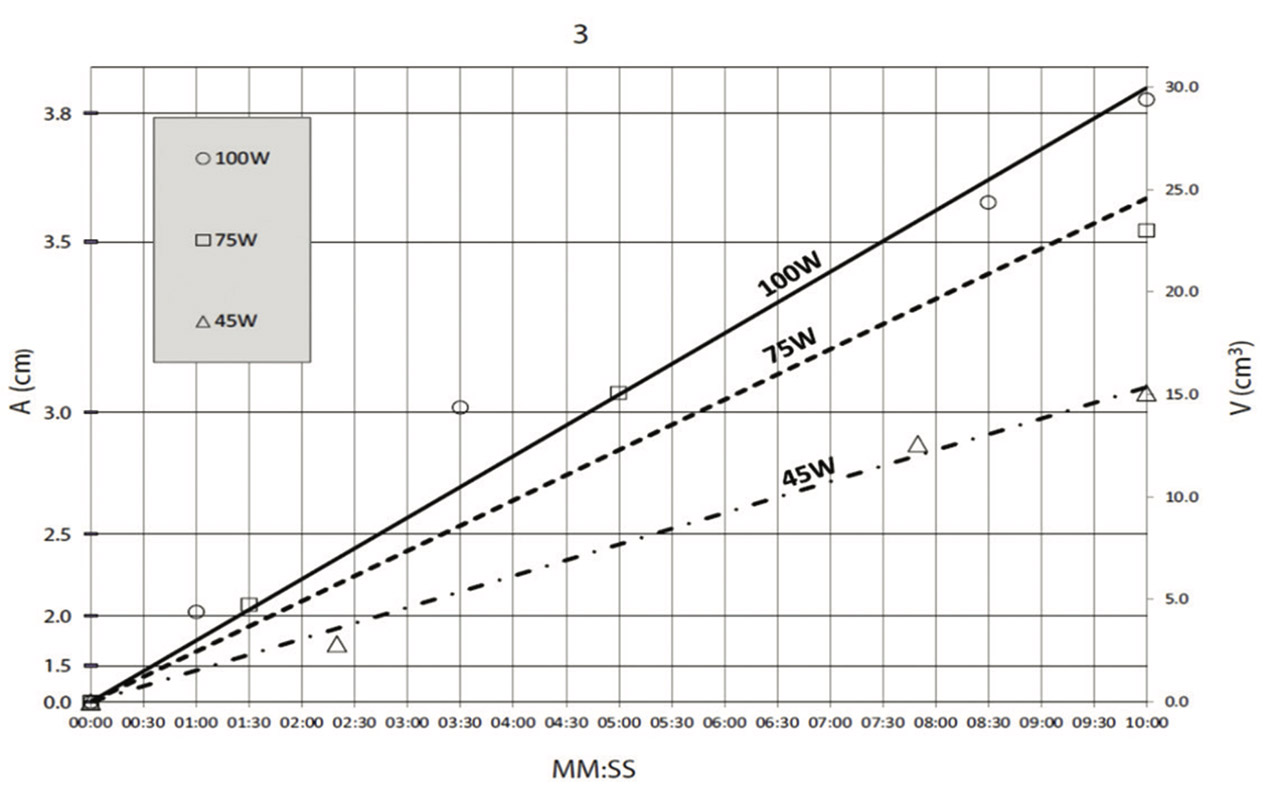
Figure 4: This graph shows the MWA power and duration in relation to the size of the lung lesion
MWA is proven to be a safe procedure but this has thefollowing possible risks and complications: pneumothorax,pleuritis, pulmonary abscess, pulmonary hemorrhage, lunginflammation, thoracic wall injury and mortality.21 In researchundertaken by Steinke et al., the rate of traumaticpneumothorax is reported to be as high as 50% noting that50% required chest drain.22 From our case studies, one out offour had an incidence of pneumothorax which was managedby intercostal chest drain.With a high mortality rate of pulmonary malignancy andincreasing number of cases of tumor recurrence, minimal invasiveprocedures are emerging especially for non-surgicalpatients as an effective treatment option.
MWA is a minimally invasive, effective treatment forvarious cases of lung cancer. This emerging technique shouldbe increasingly considered especially for patients who are notgood candidates for surgery.