Brain injury is a public health problem that can be found in every country around the world. It causes higher medical expenses, severe disability and death.1 The World Health Organization predicted that by 2020, there would be at least 10 million brain injuries. One of the main causes of brain injury is traffic accidents. In Thailand, the major cause of brain injury is also traffic accidents. This problem leads to a loss for the national health budget and shortage of working labor since many brain injury patients are from the working-age population.2
Brain injury occurs in the brain that has been affected by an impact or Stapp to the head, brain structure loss or loss of function.3 The severity of brain injury is classified into 3 levels by Glasgow coma scale assessment (GCS) ranging from mild and moderate to severe brain injury. About 70-80% of injuries recorded are mild brain injury.4-6 However, mild brain injury with a GCS score 13-15 had enhanced cerebral hemorrhage after injury, so it is necessary to assess the risk of cerebral hemorrhage, including low, moderate and high risk. The treatment depends on risk level. The patients with moder- ate and high risk need to be admitted to the hospital for 24-48 hours and low risk patients will be discharged.1,7,8
Although the injury is not severe, the patients with mild brain injury still have a 3% chance of complications, which causes disability and death.7 Symptoms include dizziness, fatigue, irritability, insomnia, problems with concentration and memory.9,10 These symptoms can be found 85% of the time in the first week after a head injury, where the symptoms will gradually subside and can be restored to normal after 3-12 months.12,13 However, it has been reported that these symptoms may be chronic,10 in which a mild traumatic brain injury with post-concussion symptoms will continue to affect everyday life, such as the inability to perform activities, decreased ability to work or study,14 which requires time to heal and can cause a negative impact on family and society. Post-concussion symptoms that have not been monitored can worsen and result in re-hospitalization caused by unplanned care, inappropriate follow-up appointments, lack of care or not being provided with sufficient advice and information to manage the symptoms that occur. Therefore, in order to receive appropriate care and to reduce the chance of return for repeated treatment, appropriate management of information and continuous monitoring are needed for mild traumatic brain patients.15
Bangkok Pattaya Hospital is a tertiary hospital, as well as a trauma center, providing standardized patient care, with mild brain injury patients making up 70-80% of all brain injury patients. However, it was found that mild brain injury patients who received treatment had severe complications and had symptoms after brain damage. The result of the analysis of caring for mild brain injury patients found that there is lack of monitoring of symptoms, a lack of competency in nurses assigned to care for patients or a lack of experience in patient care. Therefore, to reduce the gap in patient care, we have developed and implemented nursing guidelines for mild traumatic brain injury patients that provide continuous care for patients admitted to accident-emergency units. In hospitals, preparation for discharge and ongoing symptom monitoring have been introduced to reduce complications to increase patient care outcomes.
This study used a quasi-experimental design with a one-group design. Patients with mild traumatic brain injury patients treated in Bangkok Pattaya Hospital from August 2017 to February 2018 were the study participants.
The inclusion criteria were as follows:
Sample size was determined according the program G* Power version 3.1.9.2 using effect size 0.207 form the previous study,16 power of the test 0.80, and the level of significance of 0.05, obtaining sample size of 30. An additional 5% was added to allow for participants dropping out of the study, resulting in the final sample size of 36.
Instruments
The instruments used in this study were divided into 2 parts as follows:
1. Data collection tool.
1.1. Demographic and Clinical Data forms were used to collect general information about participants, including gender, age, education level, cause of injury, Glasgow coma score, CT scan result, diagnosis, history of amnesia, length of stay and follow up.
1.2. The Rivermead Post Concussion Symptoms Questionnaire (RPQ), developed by King, was employed.17,18 The interview consisted of 16 closed- ended questions about post-concussion symptoms after injury: 1) physical symptoms 2) cognitive symptoms and 3) behavioral symptoms. There were two more open-ended questions, each item using the Likert scale 0-4 points (0 = Not experienced at all, 1 = No more of a problem, 2 =Amild problem, 3 =A moderate problem, 4 = A severe problem), where higher scores indicated higher perception of post- concussion symptoms that affects daily life. In this study, the internal consistency reliability was 0.84.
1.3. The Rivermead Head Injury Follow Up Questionnaire (RHFUQ), developed by Crawford and team19, was used to assess the functional performance of the patient’s brain injury. The interview form consists of 10 closed-ended questions, divided into 3 parts: 2 daily life questions, 6 social activities, and 6 interactions and 2 work duties. There were also 2 more open- ended questions, each item using the Likert scale 0-4 points (0 = No change - I’m the same as before the injury, 1 = No recent change but still more difficult than before injury, 2 = A mild change in my ability compared to before injury, 3 = A moderate change in my ability compared to before injury, 4 = A very marked change in my ability compared to before injury), with higher scores indicating higher severity of symptoms. In this study, the internal consistency reliability was 0.82.
1.4. The interview form for patient satisfaction using nursing guidelines was adapted from the satisfaction assessment form for nursing practice guidelines for pain management in the elderly who have sustained injuries from accidents.20 The evaluation form uses a numeric rating scale (0-10) and has open-ended questions for suggestions about the use of nursing practices.
1.5. The questionnaire for management of symptoms after the brain injury, created by the researcher, is an open-ended question to describe how to manage post-concussion symptoms and the results of the management of post-concussion symptoms.
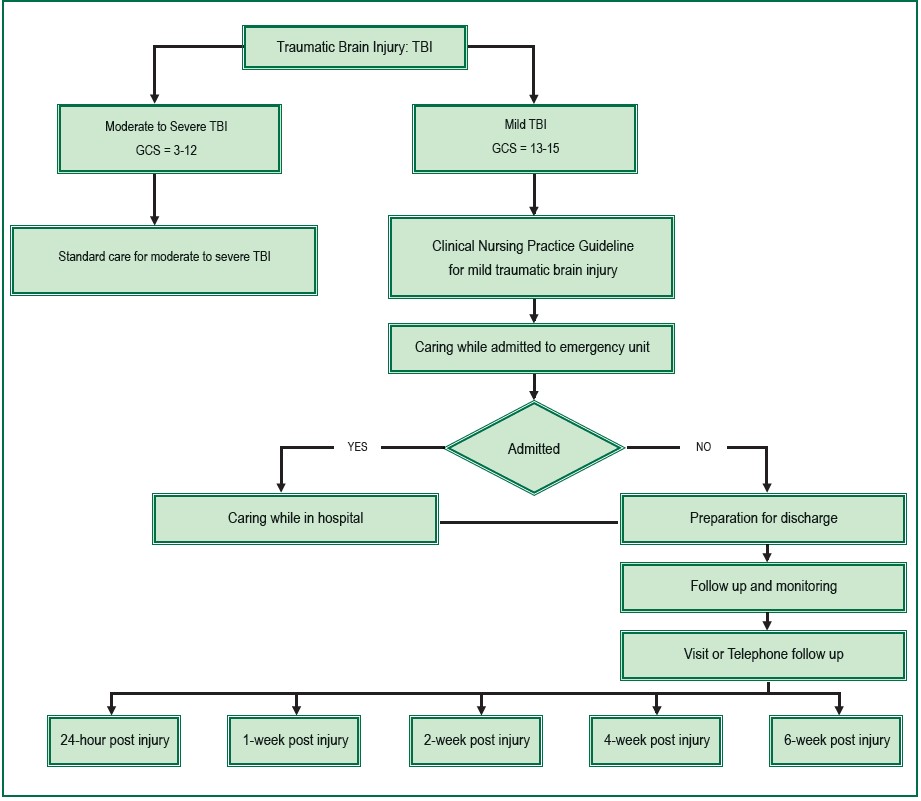
2. Clinical Nursing Practice Guideline for Mild Traumatic Brain Injury was developed based on literature review. The CNPG consists of 4 steps to take care of mild traumatic brain injury patients: 1) Care and treatment while being admitted in an accident-emergency unit in order to ensure appropriate care for patients depending on the classification of injury. This includes the screening of evaluation history, physical examination of nervous system risk assessment and classification of mild traumatic brain injury. 2) Care while in hospital for patients with mild traumatic brain injury to allow the observation symptoms according to the admission process of Bangkok Pattaya Hospital. Care processes include periodic monitoring and evaluation of patients, as well as treatments of post-con- cussion symptoms. 3) Preparation for discharge, the care planning process for discharging mild traumatic brain injury patients begins with the permission to be discharged from the hospital. 4) Monitoring and follow-ups, in order to assess post-concussion symptoms. This includes providing the appropriate information on symptom management to
patients, and scheduling regular follow-ups in order to monitor symptoms at the neuroscience center. (Figure 1) The content of CNPG was validated by 5 experts in the field of nursing and neurosurgical (0.83).
Ethical consideration
This study was approved by the Ethical Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University (No. 2560/113: ID02-60-35). The participants were approached and informed of the study details before informed consent was obtained with a right to withdraw from the study at any time. Data were kept confidentially.
Data Analysis
Descriptive statistics were used for demographic data, number of mild traumatic brain injury patients’ revisit within 28 days, satisfaction with the use of clinical nursing practice guideline for patients, post-concussion symptom, effects that interfere with daily life, dealing with post-concussion symptom, and the functional performance of the patient’s brain injury. The differences in functional performance of the patient’s brain injury were analyzed using Wilcoxon signed-rank test statistics.
The total of participants in the study was 40. Most of the group participants were female (60%), mean age was 41.6 ± 16.8 years old, married (50%), employed (35%), bachelor degree level education (47.5%), motorcycle accident (62.5%), low risk for cerebral bleeding (45%), normal CT scan result (92.5%), admitted to observe symptoms (42.5%), and average length of stay 0.77 ± 1.16 days. (Table 1).
Post-Concussion Symptoms, Interfering with Daily Activities and Management of Post-Concussion Symptoms.
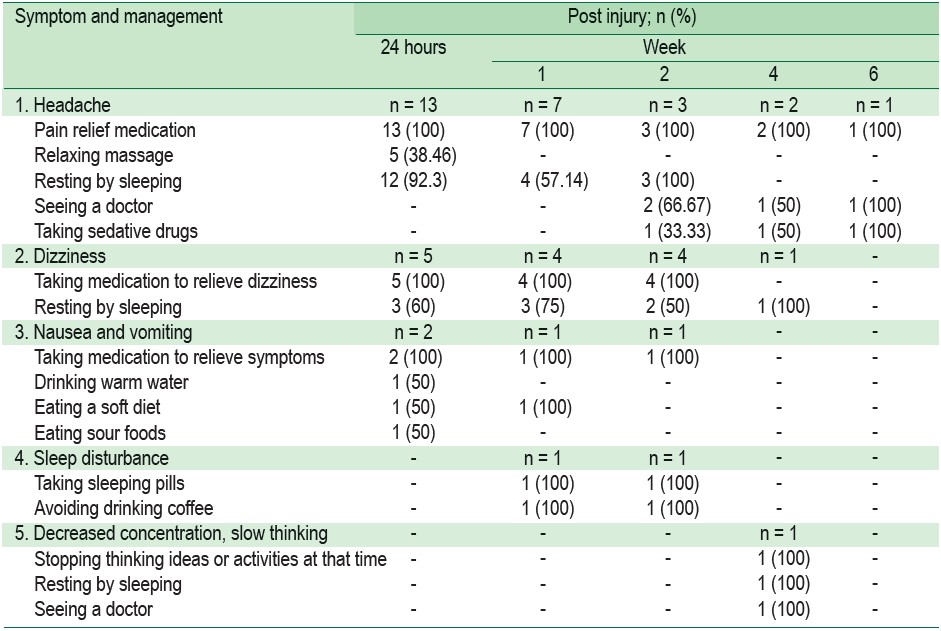
According to the follow-up post-concussion symptoms in patients with mild brain injury, at 24 hours, 1, 2, 4 and 6 weeks, found 3 common symptoms including headaches, dizziness, nausea or vomiting. These symptoms were found within 24 hours after injury, nausea and vomiting continued until 1 week, and dizziness continued until 2 weeks, while headache continued until 6 weeks. In addition, symptoms of sleep disorders were observed in 1 week and forgetfulness in 4 weeks. Participants may have more than one symptom (Table 2). Effects interfering with daily activities in mild traumatic brain injury patients were classified as follows: no interference, slight disturbance, moderate disturbance and disturbing effect. The disturbance of daily activities decreases according to the duration of symptoms after the brain has been affected (Table 3). There may be more than one way to manage symptoms. (Table 4)
Table 1: Demographics and characteristics (n = 40)
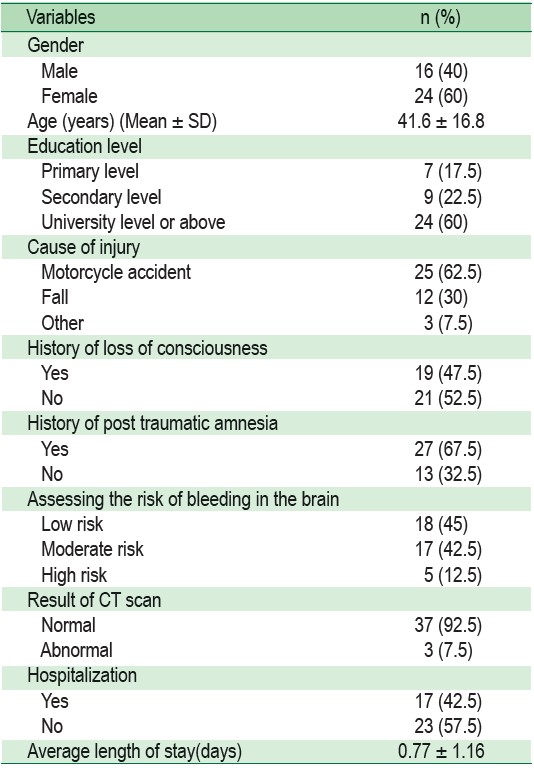
Table 2: Post-concussion symptoms and Interfering with symptoms
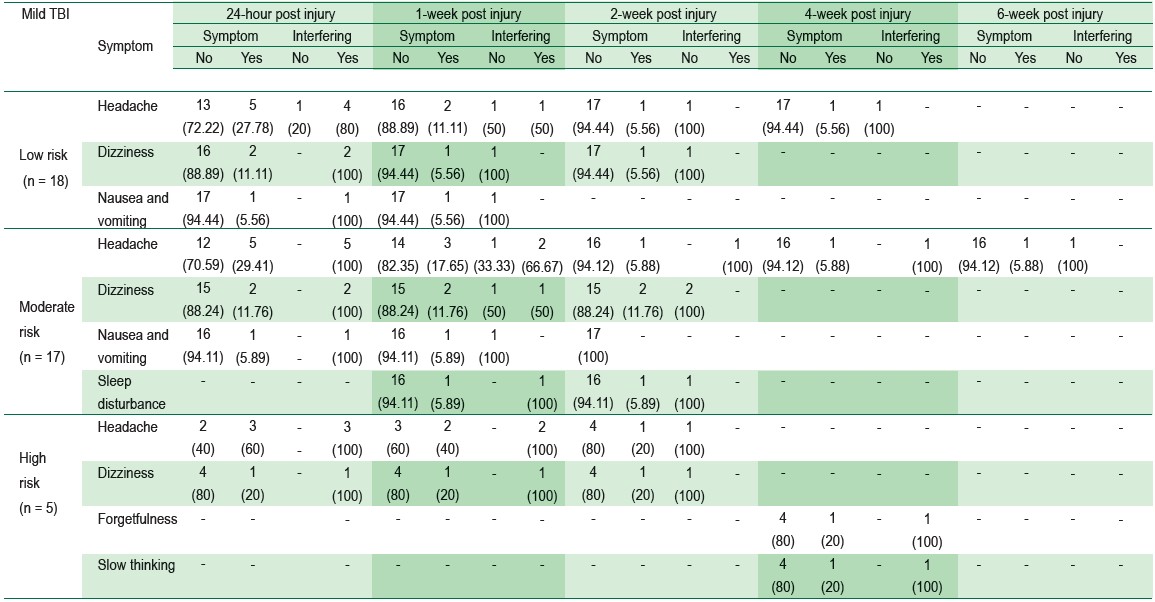 Note: Symptoms that were not found in patients include fatigue, blurred vision, blurred vision, blurred vision, decreased concentration, irritability, depression, feeling frustrated, and feeling restless.
Note: Symptoms that were not found in patients include fatigue, blurred vision, blurred vision, blurred vision, decreased concentration, irritability, depression, feeling frustrated, and feeling restless.
Table 3: Effects interfering with daily activities in mild traumatic brain injury patients
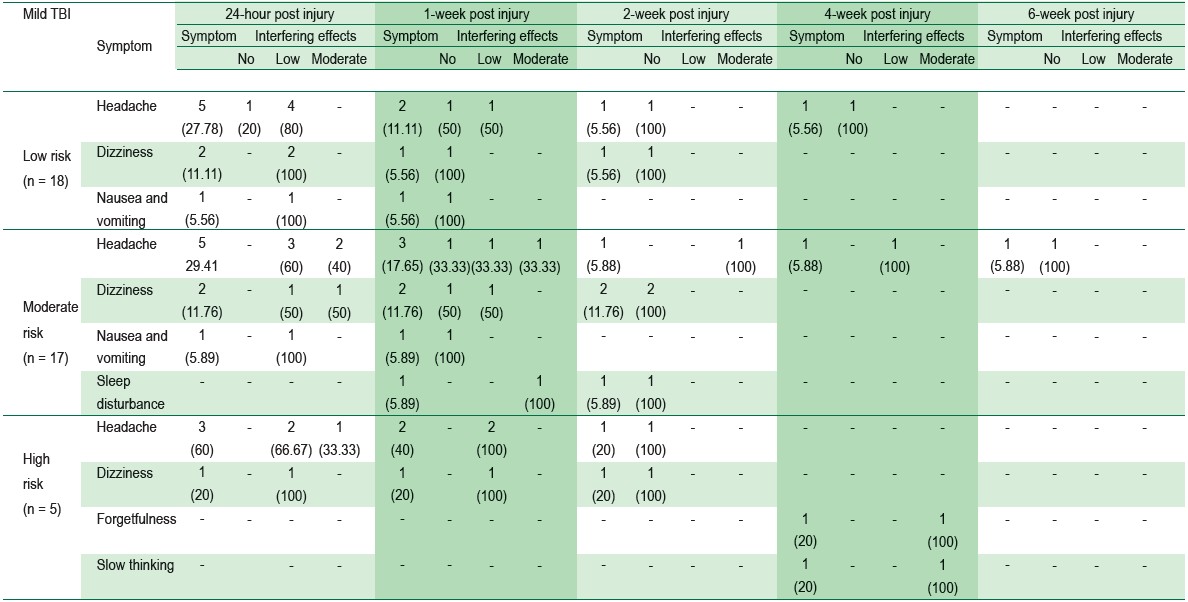 Note: Symptoms that were not found in patients include fatigue, blurred vision, blurred vision, blurred vision, decreased concentration, irritability, depression, feeling frustrated, and feeling restless
Note: Symptoms that were not found in patients include fatigue, blurred vision, blurred vision, blurred vision, decreased concentration, irritability, depression, feeling frustrated, and feeling restless
Table 4: Management of post-concussion symptoms in mild traumatic brain injury patients
The functional performance of the patient’s brain injury
It is perceived that patients with mild traumatic brain injury would have complications in their ability to perform activities in their daily lives. The results showed that the sample group has difficulty as presented in Table 5. The study found that mild traumatic brain injury patients had an average score of complications and/or changes in their ability to perform daily activities in 24 hours, and in week 1 and week 2, the average score was reduced to 0.8, 0.6 and 0.2 respectively (SD = 1.63, 1.45 and 0.63).
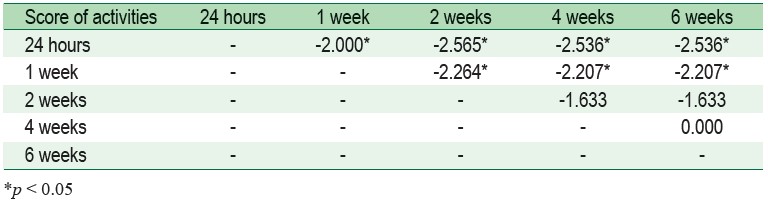
The comparison of the ability of the activities of the patients with mild traumatic brain injury within 24 hours, 1, 2, 4 and 6 weeks after brain injury showed that the ability to perform activities in patients with mild traumatic brain injury was significantly different. (X2 =26.81, p < 0.001)
Mild traumatic brain injury patients have an average score of frustration and/or changes in their ability to perform activities. Overall, in the first 24 hours, and in week 1 and week 2, the average score dropped to 0.8, 0.6 and 0.2 SD = 1.63, 1.45 and 0.63). The ability to do regular homework had an average score of frustration and/or change in the ability to perform activities in 24 hours. The maximum is 3.5 (SD = 0.77). Previous work load has an average score of frustration and/or change in the ability to perform activities standard in the 24 hours, and the maximum is 3.8 (SD = 0.84) and the ability to cope with family demands has an average score of frustration and/or change in the ability to perform activities in 24 hours and week 1, that equals 0.3 (SD = 0.15).
Table 5: Average scores and standard deviations of injury patients within 24 hours, 1, 2, 4 and 6 weeks after brain injury (n = 40)
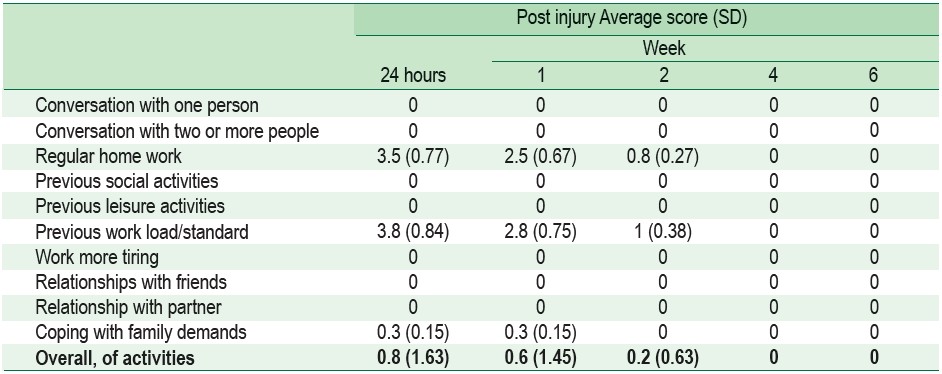
Table 6: Comparison of performance differences of the activities of patients with mild traumatic brain injury within 24 hours, 1, 2, 4 and 6 weeks after brain injury (n = 40)
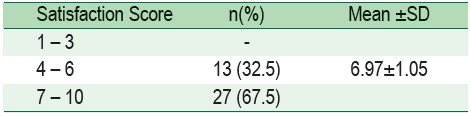
Satisfaction with the use of clinical nursing practice guidelines
Patients receiving care under the clinical nursing practice guidelines for the care of mild brain injury patients admitted in Bangkok Pattaya Hospital showed a satisfaction score in the range of 7-10 points (67.5%), with an average satisfaction score of 6.97 ± 1.05. This indicates that brain injury patients have a high level of satisfaction with care provided in accordance with the guidelines (Table 7).
According to the study, the samples had more females (60%) than males (40%). Motorbike accidents is one of the causes of brain injury. Females were more likely to have accidents than males due to the ability to make decisions, unpredictable reactions, slow response and lack of expertise in using vehicle equipment.21,22 In contrast, the causes of minor brain injuries in elderly was lower.23
Table 7: Percentage of satisfaction of mild traumatic brain injury patients with the use of clinical nursing practice guidelines. (n=40)
The results showed that the sample group had headache in the first 24 hours, with mild or moderate or severe levels. One of the subjects continued to experience headache for 6 weeks after the injury. The number and severity of symptoms gradually decreases over time, consistent with previous studies. Headache is a physical symptom in 30-80% of mild head injuries, the severity ranging from mild to moderate.10,24,25 Headache tends to decrease with time.24 However, continuous headaches can result in the development of migraines. This is because the headache in the brain injury caused the brain cells in the injured area to become inflamed, swollen, press against the blood vessels and meninges, leading to neurotransmitters and abnormal blood flow in the brain.26 Headaches will cause the brain cells to swell heavily during the first 48-72 hours after being injured.27,28 Later, the reaction to the inflammation of the body will cause water and protein to be pulled back into the blood vessels, resulting in the swelling of the brain cells gradually decreasing, improving blood circulation in the brain cells to allow more oxygen, which will subsequently decrease the severity of the headache.
All subjects with headache took paracetamol as medication. Symptoms saw improvement after patients took the drug together with getting plenty of rest and sleep. In addition, 38.46% of patients used massage methods to relax with medication and rest consistent with previous studies.29 One patient had constant headache continuously for 6 weeks, affecting their daily life on a moderate level. The researchers consulted the doctor about the pain that occurred and recommended consultation to the neurological department. The patient was diagnosed with migraine and treated with non-steroidal anti-inflammatory drugs in combination with sedative drugs, nortriptyline. Patient’s headache subsided after treatment but throughout the follow-up there was still a headache. The patient’s headache improved in the 8th week after brain injury.
In addition, it was found that 12.5% of patients had dizziness and 5% had nausea. Dizziness, nausea and vomiting originates from the inner ear which is related to balance movement. When the impact affects the signal, it can cause dizziness.30 Patients need to be evaluated for other causes of dizziness, nausea and vomiting in order to receive proper treatment. There are many ways to manage dizziness, nausea and vomiting after brain injury, including relaxation and reduced physical activity. Medication for the dizziness and nausea, stimulating environment reduction, such as color lights or balance physical therapy, and movement (vestibular rehabilitation) etc.31 Our study found that management of dizziness, nausea, and vomiting by medication was 100%, resting 60%, drank warm water 50%, ate soft diet 50% and ate sour fruit 50%. There was no nausea and vomiting in the 4thweek, and no dizziness in the 6th week.
One sleep disorder patient was found to have a continuous headache. This is due to the pathology of the head injury, resulting in abnormal secretion of serotonin and melatonin. The secretion of norepinephrine increases the activation of the reticular system, which causes the sleep and wake mechanisms to malfunction, causing a higher alert to stimuli and losing balance in the sleep cycle.32 After receiving a sedative, nortriptyline, the patient slept better. Sleep disorders disappeared within the 4th week after brain injury.
Patients can effectively manage symptoms that manifest after a traumatic brain injury. With proper preparation, mild traumatic brain injury patients will be able to perform self-care activities.
Patients experiencing symptoms after the traumatic brain injury, can deal with problems effectively. Although this depends on the patient’s knowledge preparedness and knowing how to manage the symptoms by various methods in a systematic way. Structured knowledge will help mild traumatic brain injury patients be able to perform self-care activities, consistent with a study by Paramaporn.33 As well as the use of brochures as a tool for patients to manage symptoms and prevent complications, it was also found that teaching in conjunction with the distribution of care manuals will help reduce the duration of post-concussion symptoms.34,35 Handbooks and brochures will help encourage patients to understand, memories and have the opportunity to review what they have learned, which will help reduce anxiety.
Post-concussion symptoms management will increase the functional performance of traumatic brain injury patients. The sample group had the highest average score of difficulty performing daily activities in 24 hours, and in 1 and 2 weeks, their scores decreased by 0.8, 0.6 and 0.2 (SD = 0.84, 0.75 and 0.38). When comparing the ability to perform daily activities of mild brain injury patients, it was found that the ability to perform activities significantly increased (p < 0.05) within weeks 1, 2, 4 and 6 after brain injury. During the first week after brain injury, patients had the ability to perform reduced daily activities. However, after a period of time, until the 4th week, mild traumatic brain injury patients had a better ability to perform daily activities compared to before a brain injury. This demonstrated the ability to perform daily activities in relation to post-concussion symptoms.13,15 The increase in the number and severity of post-concussion symptoms on patients caused an increase in difficulty in performing cognitive tasks, works and activities, whereas the decrease in the number and severity of the symptoms resulted in an increase in the ability to perform daily activities.24,25
Satisfaction levels of mild traumatic brain injury patients receiving care according to CNPG showed that the samples were satisfied with moderate to high levels of nursing care because the subjects were closely monitored and managed when post-concussion symptoms had occurred. Symptom monitoring and counselling for post-concussion symptoms helped reduce anxiety for the complications that occurred, increasing the ability to care for the illness, allowing a better relationship between patients and nurses, and resulting in higher satisfaction.
The results of the study showed that a successful implementation of CNPG in patients with mild traumatic brain injury, used to evaluate and monitor for post-concussion symptoms, results in effective management of post-concussion symptoms and in increased abilities post injury. Appropriate management of information and continuous monitoring are needed for mild traumatic brain patients. CNPG can improve patient outcomes by minimizing complications and enhancing the functional performance of mild traumatic brain injury patients.
The author would like to thank all the participants who took part in this important study, and all the staff at Bangkok Pattaya Hospital who supported the study.