Pulmonary nodules are common findings in radiographic images. They can be detected on a person’s annual chest x-ray, screening for lung cancer, symptomatic patients requiring diagnostic procedures, follow up images for monitoring of earlier seen nodules and for some, after undergoing treatment for infection or lung malignancy. It has been noted that solitary pulmonary nodules can be found in 0.09 to 0.2% of all chest x-rays.1
The use of chest CT scan in the early detection of lung cancer has been widely used in the past decade. Lung nodules are easily discovered because of the higher resolution compared to chest x-ray, prompting physicians to facilitate further investigation for immediate and accurate diagnosis and treatment. The increased utilization of chest CT scan can be associated with the success of the National Lung Screening Trial (NLST), that reported a 20% reduction in lung cancer death in a high-risk cohort of patients screened in the US.2 However, it has not been proven if the NLST reports are also applicable to other settings especially in Asian countries where tuberculosis is common.3,4
Prompt screening of lung nodules is critical for prognosis since the management of malignant and benign nodules is completely different. It was reported that the occurrence of malignancy in solitary pulmonary nodules ranges from 10-70% 5,6 while benign lesions caused by infectious granulomas consist of 80% and hamartomas about 10%.7, 8 which makes diagnosis a challenge among clinicians.9
The objective of early lung cancer screening is to lessen lung cancer deaths by prompt diagnosis of malignancy at a localized stage allowing effective treatment. While other clinicians form their plan of care by following specific guidelines like the application of American College of Chest Physicians (ACCP) guidelines in Asia,10 many physicians still conclude their impression subjectively, by intuition or based on their experiences which result to improper diagnosis.11
When a lesion is discovered, the main goal is to identify if it is benign or malignant. Before any diagnostic tests should be performed, the risk of malignancy should be computed using one of the established lung cancer probability formulas to find out the yield of clinical probability of malignancy. In this study, we applied the Mayo Clinic model which utilizes information such as a person’s age, smoking history (current or former or never), extra-thoracic cancer more than 5 years prior, size of nodule in mm, spiculated morphology and upper lobe lung location.11
Thailand remains one of the high-TB burden countries.12 TB and lung cancer have common symptoms, radiological similarities 13 and these can occur simultaneously or sequentially.14-17 In our previous article, we reported nodules/ mass measuring 4.5- 11 mm in our institution all caused by TB.18 To further expound on the connection of lung nodule characteristics and diagnosis, we used the Mayo Clinic formula to find out if this is an effective and applicable tool in determining the probability of lung cancer in TB-endemic countries.
We retrospectively collected and reviewed the medical records of 54 patients at the Bangkok Hospital Medical Center who underwent a chest CT scan and were identified to have lung nodules/mass, measuring 4.5-88 mm between 2012 and 2014. Of the 54 individuals, 100% agreed and consented to undergo further investigation such as Fiberoptic bronchoscopy (FOB), Endobronchial Ultrasound (EBUS), Electromagnetic Navigation Bronchoscopy (ENB) and Video Assisted Thoracoscopic Surgery (VATS) to establish final tissue diagnosis. Specimens were tested for AFB stain, PCR-TB, cytopathology and fluid culture and sensitivity.
Clinical data gathered were patient age, gender (male or female), race (Asian or Non-Asian), smoking history (smoker, previous smoker or never having smoked), extra-thoracic cancer for more than 5 years prior to the consultation, lung nodule/mass location (upper, middle, lower) and spiculated morphology.
Lung nodule/ mass characteristics were obtained from the official reports of radiologists. Extra-thoracic cancer history was positive among nine patients (17%) but they were included as they were on complete remission and the results did not make a significant difference. The variables obtained were then used to compute the lung cancer probability using the Mayo Clinic formula.
The Mayo Clinic model is described as follows: Pre-test probability of a malignant solitary pulmonary nodule (SPN) = ex/ (1+ex). Where x = -6.8272+ (0.0391 x age) + (0.7917 x smoking history) + (1.3388 x cancer history) + (0.1274 x diameter of nodules/ mass) + (1.0407 x spiculation) + (0.7838 x upper lobe), e is the natural logarithm. Corresponding points are 1 for smoker or previous smoker and 0 for non-smoker, 1 for yes or 0 for cancer history, spiculation and upper lobe variables. Watchful waiting is recommended for scores of <3%, biopsy for 35 to 68% and surgery is advised for patients with 68% scores.11,19 While all our participants had undergone pulmonary nodule or tumor analysis through biopsy or surgery, we evaluated the accuracy of the Mayo Clinic formula for estimating the probability of lung cancer by computing and then comparing the lung cancer probability result versus the final diagnosis.
A case example is illustrated as follows: A 60-year old male patient came for consultation due to an incidental finding of a lung nodule. Chest CT scan reported a 13 mm spiculated nodule abuts the bronchus to posterior segment of right upper lobe. He was a heavy smoker with no known underlying condition. The following data were gathered: age: 60, smoking history: yes (1), cancer history: no (0), diameter of nodule: 13 mm, spiculation: yes (1), and upper lobe: yes (1)
Probability score of lung nodule: e is approximately 2.71828
= 2.71828(-6.8272+ (0.0391 x 60) + (0.7917 x 1) + (1.3388 x 0) + (0.1274 x 13) + (1.0407 x 1) + (0.7838 x 1)/1 + 2.71828(-6.8272+ (0.0391 x 60) + (0.7917 x 1) + (1.3388 x 0) + (0.1274 x 13) + (1.0407 x 1) + (0.7838 x 1)
= 0.81155753092 / (1+0.81155753092)
= 0.44798882567 or 44.8%
From this computation, we were able to obtain a score of 44.8%, suggesting tissue biopsy of lung nodule according to Mayo clinic lung cancer probability formula. Lung nodule biopsy was done and pathology result reported adenocarcinoma.
We described accuracy by comparing the predicted probability of malignancy with the final diagnosis.
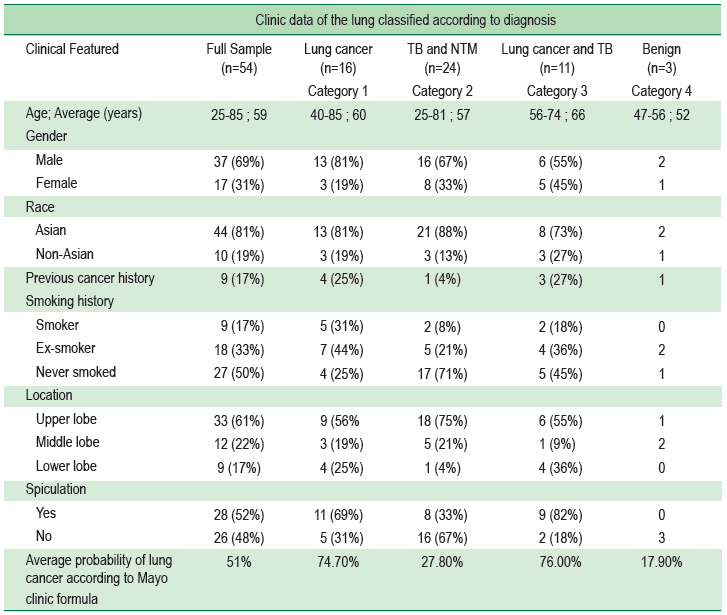
Pathological results
For the 54 patients with a confirmed final diagnosis, lung cancer was found in 16 patients, tuberculosis with non-tuberculous mycobacteria (NTM) infection in 24 patients, 11 cases were diagnosed with lung cancer with TB and 3 cases appeared to be a benign tumor.
Average probability of lung cancer according to Mayo Clinic formula divided into 4 categories
For the first category, patients diagnosed of lung cancer, the result from the Mayo Clinic formula was 74.7% probability. Category 2 (TB and NTM infection) lung cancer probability was 27.8%, category 3 (lung cancer and TB) was 76% and category 4 (benign) was 17.9%.
Table 1: Sample characteristics and comparison of the lung cancer probability of patients divided into four categories based on final diagnosis.
The Mayo Clinic probability equation was formulated when Swensen et al. reviewed medical information of 629 individuals at the Mayo Clinic with pulmonary nodules/ tumors that measured 4 to 30 mm in diameter in 1984 and 1986. Through examination of data, they were able to identify six variables that affect prediction of lung cancer. These are: age, smoking history, extra-thoracic cancer history of more than 5 years prior to tissue study, nodule or tumor diameter, upper lobe location and spiculated border of nodule/ tumor. 19 This information was then analyzed to formulate the Mayo Clinic lung cancer probability equation.
In our study, the full sample of 54 patients obtained an average of 51% lung cancer probability which means that in every individual, considering the clinical data obtained, the possible impression could be either lung cancer or infection (TB and NTM). Lung infection specifically TB can mimic lung cancer radiologically and clinically.13, 20-22 In these cases, lung tissue should be obtained by biopsy to acquire precise diagnosis.9 In this study, 100% of patients underwent biopsy or surgery to obtain tissue for cytopathology studies.
The accuracy was validated by collecting patient history and lung nodule characteristics forming variables that were then applied to the Mayo Clinic formula. The average probability of each diagnosis was then compared and evaluated.
The Mayo Clinic probability result for category 1: lung cancer is 74.7%, category 2: TB and NTM is 27.80%, category 3: lung cancer and TB is 76% and category 4: benign diagnosis is 17.90%. It is evident that the groups with pulmonary neoplasms have a significantly higher percentage of probability compared to those with infection only. This shows that the Mayo Clinic formula is an effective tool when examining individuals for malignancy even in TB endemic areas considering also that TB and lung neoplasms can occur at the same time. 14, 21, 23
There are two other mathematical prediction models used for lung nodule malignancy probability. These are the Veteran Affairs (VA model) and Peking University (PU) model. A number of studies have validated the efficacy of these formulas including the Mayo Clinic formula.11, 19, 24 Zhang X et al.,11 concluded that physicians should use a predictive formula based on the local occurrence of cancer. They further elaborated that the PU model should be applied in China and similar areas. On the other hand, E M Shultz et al. stated that according to their review, both the accuracy of the Mayo Clinic and VA models are enough for the formulas to be used clinically but should not be used as stand-alone test.19
EM Shultz et al.19 also recommended that clinicians should weigh the consequences of a false positive diagnosis compared with those of a false negative diagnosis before choosing a probability formula. To support this statement, we present a case of a 25-year old male, single patient, who came for consultation due to mild dyspnea, cough with greenish sputum, hemoptysis and hoarseness of voice. He is a non-smoker with no history of cancer. His chest CT scan revealed a 72 mm well-defined lobulated mass at the left upper lobe. His Mayo Clinic probability score was 98.38%. Quantiferon TB was negative. He underwent EBUS and result was chronic granulomatous lymphadenitis. Medication treatment was prescribed and a year later, his chest x ray revealed normal results. This shows that probability formulas should only to be used as a guide and not as a stand-alone factor when making clinical judgments, although, in this particular instance, this could arguably be seen as an isolated case.
One of the limitations of our study is that we were not able to compare the use of the Mayo Clinic formula with the aforementioned prediction models. As this is a retrospective study, several data such as number of years since quitting smoking and family history of cancer are not available in some of our subjects’ records. Another limitation is that we collected the nodule characteristics based on the official report of radiologists rather than examining the CT images ourselves.
We also have to consider that while our facility has the capacity to detect and record many tuberculosis patients, the data collected was limited to the private sector only, resulting in restrictions on information and statistics available from public hospitals.
To summarize, individuals with a lung cancer probability score of more than 3% should undergo a lung nodule biopsy to determine the proper diagnosis. Watchful waiting should not be considered as this may delay treatment and management. As elaborated from our data, lung cancer patients illustrated a higher score of 74.7% (lung cancer) and 76% (lung cancer and TB) which emphasizes that the application of the Mayo Clinic formula can be useful in TB endemic areas.
The Mayo Clinic formula is an effective and useful tool in predicting the probability of lung cancer even in Asian countries where TB is endemic. By using this model, physicians are provided with an aide in making a better plan of care and treatment. The Mayo Clinic probability score can help in choosing the proper diagnostic procedure and interpretation of subsequent test results. While this tool seems effective in the majority of our cases, one should still remember that decision-making should not be based entirely on the result of this lung probability formula.
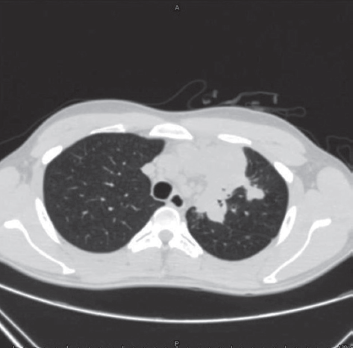
Figure 1: Chest CT scan of a patient with 72 mm mass at left upper lobe lung.
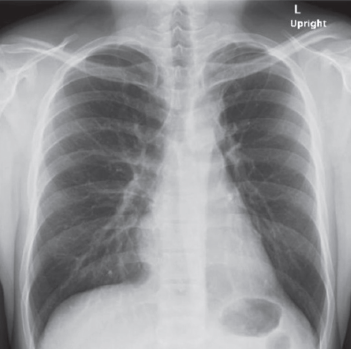
Figure 2: Chest x-ray of patient after 1 year of treatment