Advances in medical technology and increases in the clinical complexity of diseases have led to a greater need for medical care specialization. In Thailand, a general practitioner is a person who has completed six years of higher education in medicine. Meanwhile, medical specialists are those who have had further training for a period of two to six years in a special field. Although a general practitioner may provide a wide range of clinical care services to patients, a medical specialist is still essential for a more complicated clinical condition. For instance, Edwards et al.,1 explored the trends in patient, physician, and visit characteristics and compared the quality of visits between generalists and specialists; they found that quality of care for cardiovascular disease was better in visits to cardiologists than in visits to generalists. Likewise, Go et al.,2 found that patients with coronary arterial diseases or heart failure in the United States who were treated by cardiologists were more likely to receive evidence-based care and probably have better outcomes such as lower short-term readmission rates. Bateman and Fonagy3 found that patients with Borderline Personality Disorder (BPD) significant Axis II comorbidity did better with specialist treatment.
Some patients might prefer specialists to generalists because of a strong belief in relatively better clinical outcomes.4-7 Although many medical conditions are not complicated and, therefore, are manageable by public healthcare services, a considerable number of patients are willing to pay for medical attention by medical specialists in a private hospital. The rise of medical tourism reflected not only how much smaller the world has become in the globalization era, but also partly reflected the extent to which patients who distrusted the healthcare systems of their home countries were willing to invest in getting specialized medical care abroad.
Despite the clinical benefits and patient preference mentioned herein, both the number and distribution of medical specialists in the public sector have raised concerns, especially in developing countries. In Thailand, for example, a severe shortage of both generalists and specialists, particularly in the rural areas, has been reported8 as well as an “internal brain drain” out of the public sector, potentially because of the growth of the private sector. 9,10
Meyer et al.11 found that indications for the procedures varied significantly between generalists and specialists. Specialists tended to have sicker or more complex patients as demonstrated by the more serious indications and higher complexity of the procedures performed. Carmen et al.12 found that larger hospitals, such as private hospitals, had higher average case mix index (CMI), consistent with a marker of disease severity. Thus, hospitals with more specialists will have more clinically complex patients.
Patient preference in how the provision of health care is provided is an important consideration. Practical and pressing healthcare concerns on physician gender may be related to patients’ willingness to seek medical care and their satisfaction with medical care.13 A physician shortage is especially problematic in highly gendered fields, such as general surgery.14 Therefore, the gender imbalance across specialties in medicine has implications on not only the theoretical causes of gender inequality but also the needs within the profession and its communities. In addition, Muslim women, if given the option, are more likely to prefer female doctors to their male counterparts.15 In some specialties, such as gynecology, breast surgery, and urology, there is a preference for a female doctor, especially among female patients, if given the choice.16-20
According to the “World Bank Report East Asia’s Changing Urban Landscape: Measuring a Decade of Spatial Growth,” urban growth in Thailand has been dominated by the Bangkok urban area, which was the fifth-largest in South East Asia in terms of area and the ninth-largest in terms of its population, which was approaching 10 million, in 2010.21 Therefore, we define the urban area as the Bangkok Metropolitan region and the remaining area as the rural area. Urban and rural areas vary in their utilization of medical care. Previous studies have reported that healthcare is generally considered to be more highly valued in urban areas than in rural areas.8,10,22,23 The United Nations forecasts that the urbanization rate of Thailand will increase from 35.6% in 2015 to 40.7% in 2025. This shows that urban expansion is an opportunity for the expansion of medical services to regional provinces that are rapidly expanding when compared to the need in the Bangkok Metropolitan area. 24
Given the increase in the number of doctors in Thailand during the past decade, maximizing the allocative efficiency of medical specialist distribution has been a more challenging research question. The limited availability of public sector data results in the need for alternative sources of scientific evidence.
As the largest network of private hospitals in Thailand, the Bangkok Dusit Medical Services (BDMS) needed to make a strategic move to maximize the allocative efficiency of general practitioners and medical specialists in the network of 32 hospitals throughout the country. A better understanding of how medical specialists were distributed would not only be beneficial for other private hospital networks, but the findings might also be generalizable to the public sector in Thailand and elsewhere.
This study analyzed the BDMS Medical Doctor (BDMS-MD) database during 2012- 2016, which contains demographics, clinical credentials, and practice characteristics of all medical doctors (MDs) who work in 32 hospitals in 6 subgroups: the Bangkok Central (Group 1: 5 hospitals), the Samitivej and BNH (Group 2: 5 hospitals), the Bangkok Eastern (Group 3: 4 hospitals), the Bangkok Northern (Group 4: 7 hospitals), the Phayathai and Paolo Memorial (Group 5: 8 hospitals), and the Bangkok Southern (Group 6: 3 hospitals).
Data that met the following inclusion criteria were included in the analysis:
1. The hospital was part of BDMS management for at least a year. 2. The hospital had data on the active doctor as required such as gender, age, education, specialty and job
experience.
3. The Hospital Information System (HIS) had kept CMI
and workload data.
4. The hospital had dedicated staff who collected and
submitted data to headquarters on a monthly basis. The responsible person met the required criteria as follows: be in a position to authorize to handle or see doctor’s information.
Incomplete and/or unreliable data were excluded
A total of 32 hospitals were studied in this research as assessment of unsatisfactory data quality resulted in the exclu- sion of 6 hospitals from the analysis.
Doctor’s capability evaluation
Case Mix Index (CMI): The CMI is the average relative DRG weight of a hospital’s inpatient discharges, calculated by summing the Medicare Severity-Diagnosis Related Group (MS-DRG) weight for each discharge and dividing the total by the number of discharges. The CMI reflects the diversity, clinical complexity, and resource needs of all the patients in the hospital. A higher CMI indicates a more complex and resource-intensive caseload.25 We exported data from HIS to an excel file.
Workload: Workload points for the MDs were measured by summing up the number of OPD visits, IPD days, and OR cases.
Instrument
1. Case record forms were used to collect demographics, clinical credentials, and practice characteristics of all medical doctors
2. Dummy tables were used to test reliability by test and retest method
Data Collection
Monthly data were submitted by individual hospitals to the main database, then we exported them to excel, then we checked the reliability of data by test and retest method for intra-rater reliability and record data in case record forms, by mapping data with the care provider code, for case mapping and records in the case record forms.
Data Analysis
Descriptive statistics were used for analyzing demographics, clinical credentials, and practice characteristics of the medical doctors. A Chi-square test was used to compare the proportion of generalists and medical specialists of each group and the proportion of urban and rural of each specialty, whereas independent t-test was used for case-mix index in generalist and specialist. Analysis of variance (ANOVA) was used to examine the differences of case mix index among the groups of BDMS. Statistical analysis was performed on the computerized statistical program (Stata/ MP Version 14).
Data from 9,909 MDs were analyzed. The mean age of MDs was 40.20 years, and 57.49% were male (Table 1). There were 1,539 GPs and 8,370 medical specialists. Most specialists (74.22%) worked in the Bangkok Metropolitan area and the central region (Urban) of Thailand (Figure 1).
The top 5 medical specialists comprised internists 19.78% (1,656 MDs), followed by pediatricians (11.60%; 971 MDs), orthopedic surgeons (9.04%; 757 MDs), obstetricians /gynecologists (8.85%; 741 MDs), and surgeons (8.16%, 683 MDs), respectively (Table 2). Gender of the MDs varied across specialties (Table 3). Although there were more female MDs in the central region of Thailand, by region, female obstetricians, breast surgeons, and urologists were in short supply in the south of Thailand based on the proportion of female doctors to the number of Muslim populations.
A significant statistic variation in the urban-to-rural proportion across medical specialties was revealed in Figure 2 (p < 0.01).
Table 1 : Demographics, Clinical Credentials and Practice Characteristics of 9,909 Medical Doctors in 32 hospitals
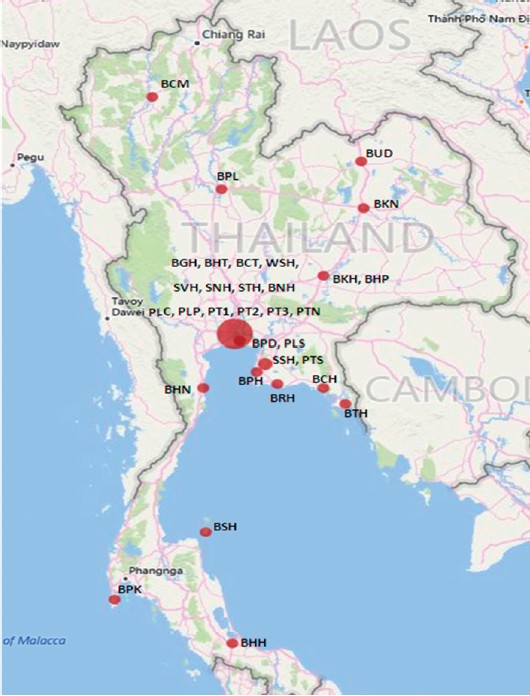
Figure 1: Geographical Location of 9,909 Medical Doctors in 32 Hospitals
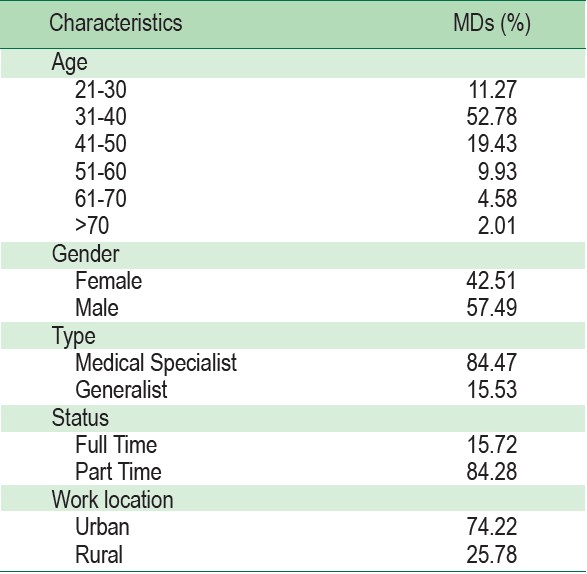
Table 2 : Medical Specialists by Specialties
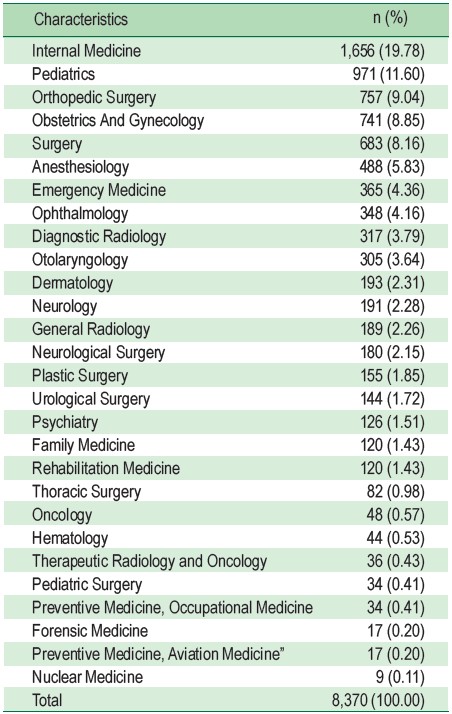
Table 3 : Gender Variation across Medical Specialties that concern on gender.
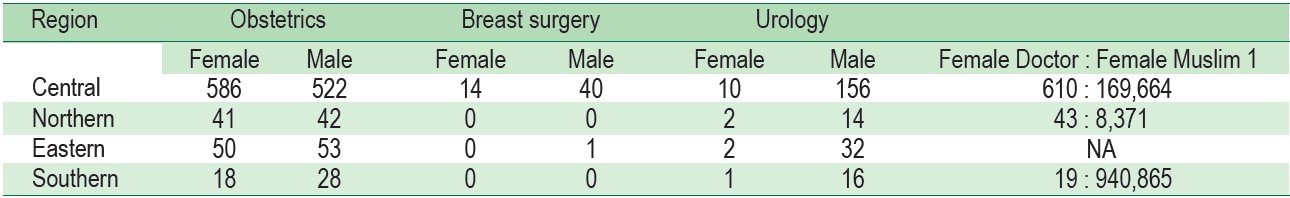
Figure 2 : Variation of Work Location across Medical Specialties
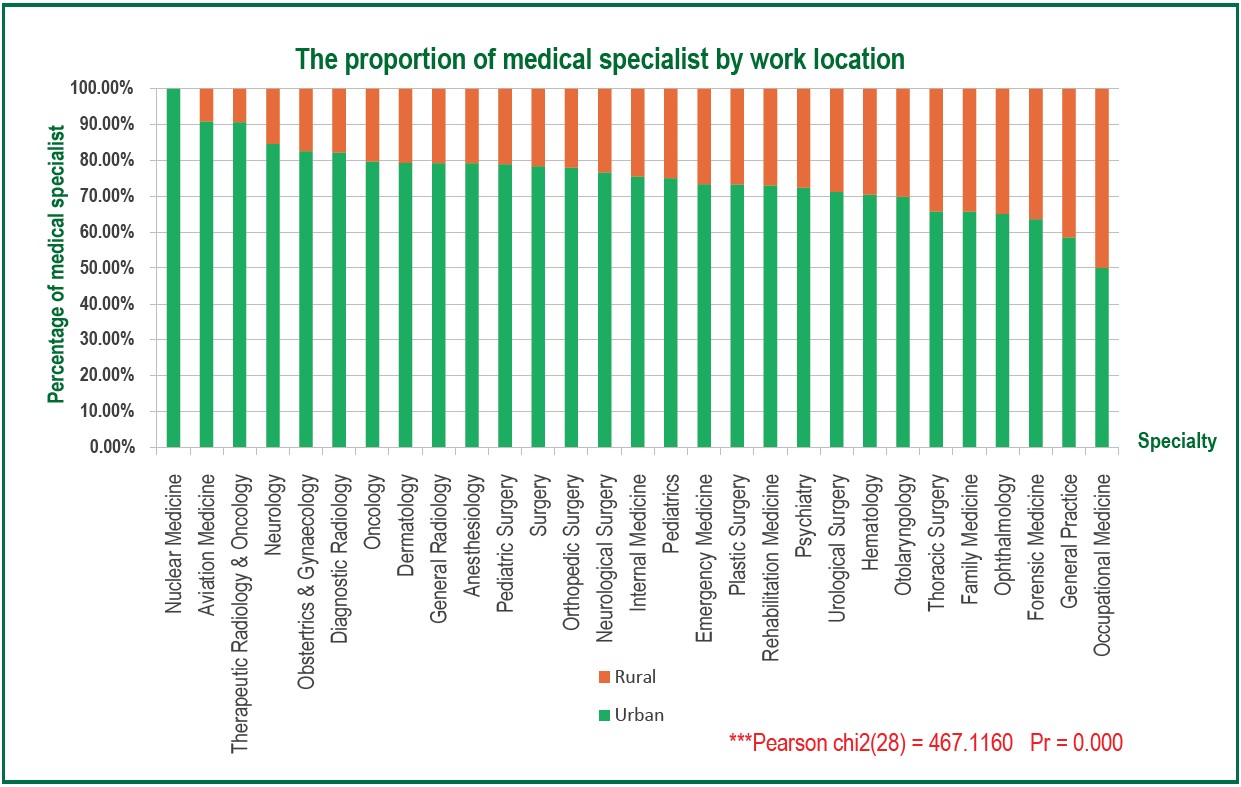
Figure 3 : The Proportion of Medical Specialists to General Practitioners and Case Mix Index
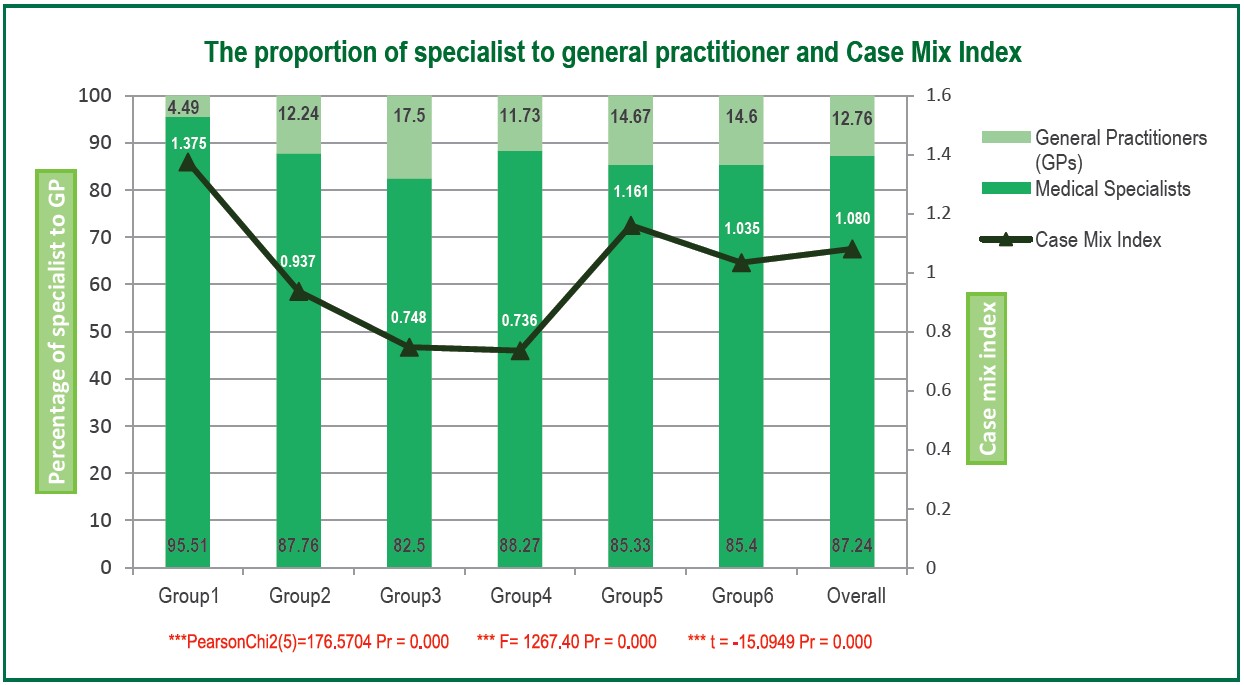
The proportion of medical specialists to general practitioners varied significantly across network subgroups (p < 0.01), ranging from 96:4 to 83:17; there was a correlation between the ratio of specialists in Group 1 and its high CMI (Figure 3). In addition, the results show that specialists had a statistically significantly higher mean score on the CMI (1.096) than GPs (0.970) based on the t-test (p < 0.01).
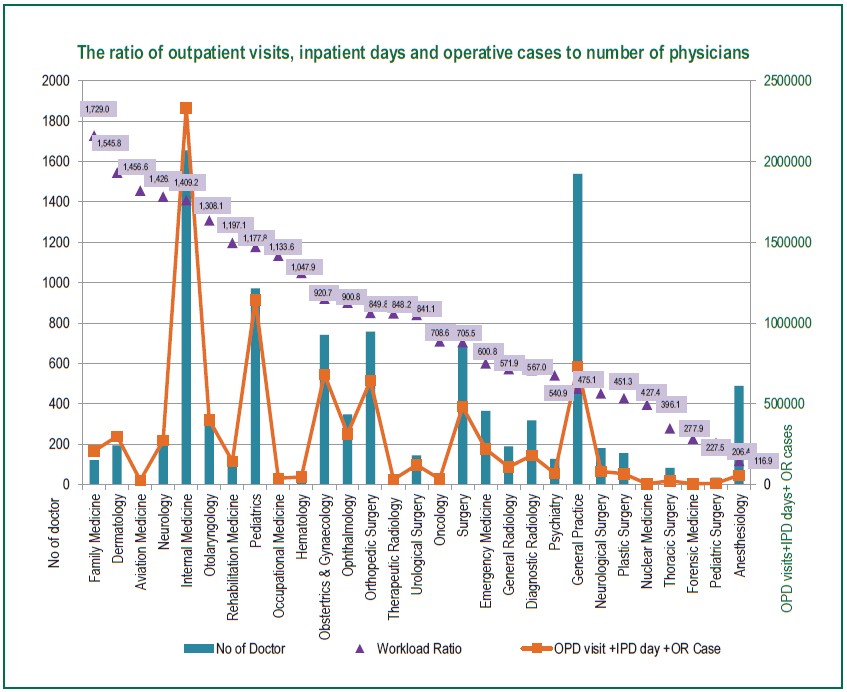
Family physicians had the highest workload (1 MD: 1,729 points), followed by dermatologists (1 MD: 1,546 points), aviation physicians (1 MD: 1,457 points), neurologists (1 MD: 1,427 points), and internists (1 MD: 1,409 points) (Figure 4)
Figure 4 : Workload Points (OPD visits, IPD days and OR cases) and Number of MD
The finding from this study shows that the private hospital network in Thailand utilized many more medical specialists than GPs. It is possible that patients come to the private hospital specifically for a particular treatment that is unique to the institution. Combining customer service with specialist physicians making treatment plan decisions would decrease the risk of a lawsuit. Research validates that specialist physicians give proper treatment when compared to general practitioners. 1,7
Regarding the proportion of specialists to GPs, the proportion was significantly higher in Group-One hospitals compared to the other groups. Hospitals in this group are located in the central region and require a higher number of specialized doctors to meet the demand of patients. This is also related to the complexity of the diseases that they treat, as shown by the CMI.
In the private sector, most specialists work in urban areas, which is comparable to the public sector. 8, 10 This raises the concern in this study as BDMS hospitals are located in urban areas, and the definition of urban in this study was located in the Bangkok Metropolitan region. There may not be a need for medical specialists to work in rural areas.
When we consider the role of the caregiver’s gender, it is crucial to take into account the relationship between the assigned physicians to match the needs of the patient; for example, certain specialties require cultural/sexually sensitive examinations, such as obstetrics and gynecology or breast care. In Thailand, it is considered a cultural transgression and may be inappropriate for female patients to be treated by male physicians. Furthermore, some religions, do not allow a non-husband to touch a female. Indeed, in some countries, it is against the law. The proportion of Muslims in Thailand is high in some regions, and the results indicate that female obstetricians, breast surgeons, and urologists are in short supply in the southern part of Thailand (due to the low proportion of female doctors to the Muslim population).
Accordingly, nuclear medicine, aviation medicine, and therapeutic radiology and oncology are ranked in the top three and are concentrated in urban areas, where more advanced equipment and more cases are available for them to practice their specialty.
The unequal distribution and an insufficient number of professionals in the health workforce remain major problems in rural areas of Thailand. In the private sector, the results showed that the ratios of some specialties were low, so we can conclude that the shortage of medical specialists found in the private sector is the same as the public sector. 10
The Group One CMI was the highest, reflecting that its patients were more complicated or severe, which led to a high ratio of specialists to generalists. Surprisingly, in Group Five, which had the second highest CMI among all groups, ranked fifth in terms of its ratio of specialists to generalists. This might be because most hospitals in this group provided services for Social Security patients.
An analysis of workload by OPD visits, IPD days, and OR cases showed that family internists, dermatologists, aviation internists, neurologists, and internists had the highest workload. This result could possibly be confirmed in the BDMS network hospitals because the strategic direction of hospitals depended on the network, which would influence the medical specialties required.
Looking at the workload will help identify which specialty is still needed in affiliated hospitals in the network. To manage the scarcity problem in a certain specialty, simple recruitment may not be good enough as there is a limited number of specialists.
The reference ratio of the proportion of physicians per population in this study is based on BDMS data. Further study in both private and public sector hospitals should be conducted to compare and validate the workload of medical specialists in Thailand.
The BDMS private hospital network in Thailand utilized many more medical specialists than GPs. The inequitable distribution of medical specialists can still be found in the private sector, despite the more flexible human resource management than in the public sector. From this study, we suggest providing scholarships for physicians to study and be trained as specialized care may be the only solution for the problem. Furthermore, further research should study other private hospital networks or public sectors.
This study was funded by a research grant from Bangkok Dusit Medical Services PCL. The authors would like to thank the executives for their kind cooperation in supplying the information.
The authors declare no conflict of interest.