The meniscus of the knee has several important biomechanicalfunctions, the most important of which is load transmission andshock absorption.2 By converting the axial load to a radiallydirected force or hoop stress, the meniscus reduces wear on the hyalinearticular cartilage.3 The meniscus roots describe the insertions of theanterior and posterior meniscal horns on the tibial plateau.4,5 These structuresare critical for meniscal function since they prevent meniscus extrusionunder axial load, thereby converting axial load to a radially directed force(so-called hoop stress).6,7
Meniscus insufficiency, resulting from a posterior root tear, increases jointcontact pressures,8 especially with concomitant meniscofemoral ligament(MFL) disruption,9,10 leading to articular cartilage degeneration over time.
According to the study by Krych AJ et al.,1 there was a high rate ofmissed posterior lateral meniscus root tears ( LMPRT) on preoperative MRIreported. This retrospective cohort study reported 45 consecutive patientswith arthroscopically confirmed LMPRTs between 2010 and 2017. Of these,only 15 of 45 LMPRTs (33%) were initially diagnosed on preoperative MRI.
LaPrade et al.,11 reported a sensitivity of 0.600 (95% CI, 0.281-0.860)and a positive predictive value of 0.181 (95% CI, 0.085-0.261) for thediagnosis of LMPRTs on 3-T MRI by a blinded fellowship-trainedmusculoskeletal radiologist. They conclude sensitivity was higher formedial root tears, indicating a higher risk of missing lateral root tears onMRI. Imaging has an important role in identifying meniscus posterior hornroot tears, however, some root tears may not be identified until arthroscopy.
A 37-year old Italian man suffered from a twisiting accident at the rightknee 2 days before admission. He presented with right knee pain withswelling, and he was unable to walk and extend his right knee .
Physical examination shown as below
Right Knee: Range of motion : 15-140 (extension Lag 15 degree).Lachmann test was positive. Anterior drawer test was positive 3+ with noend point. Pivot shift test unable to evaluate due to pain.
MRI of the right knee was requested after fully completedhistory record was obtained and physical examination. The resultof the MRI from the Radiologist reveals complete tear of ACLat mid to femoral insertion and normal morphology and signalintensity of the menisci and bone bruise at the posteriorlateral tibial plateau.
Arthroscopy findings revealed complete ruptured ACL(Figure 1), femoral insertion and medial meiscus was normal,at the latereal meniscus a posterior root tear from the tibialinsertion was found (Figure 2). An arthroscopic ACLreconstruction (Figure 3) was performed to repair the lateralmeniscus posterior root tear by pullout sutured technique(Figure 4).
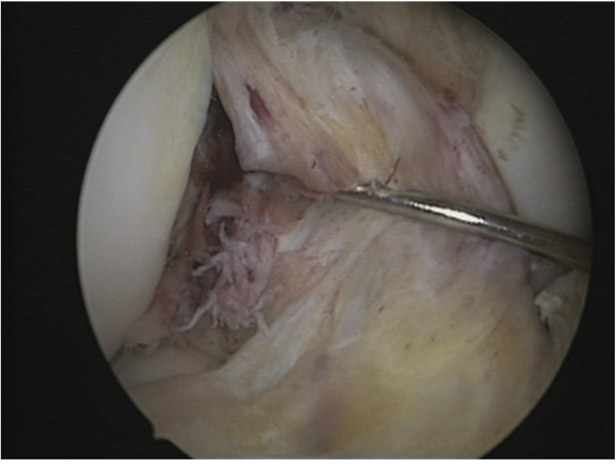
Figure 1: Complete tear of anterior cruciate ligament(ACL).
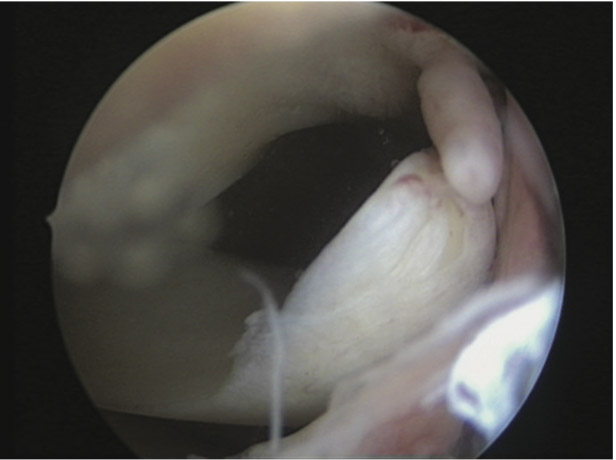
Figure 2: Arthroscopy findings reveal lateral meniscusposterior root torn from the tibial insertion.
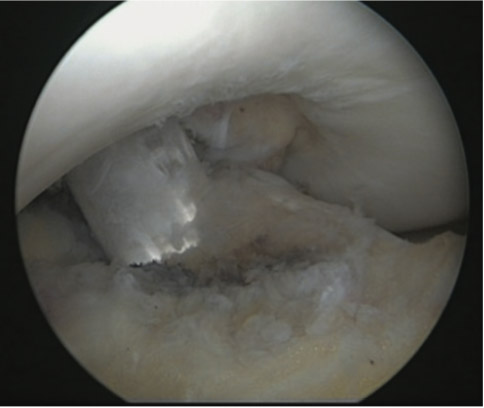
Figure 3: After anterior cruciate ligament (ACL) reconstruction.
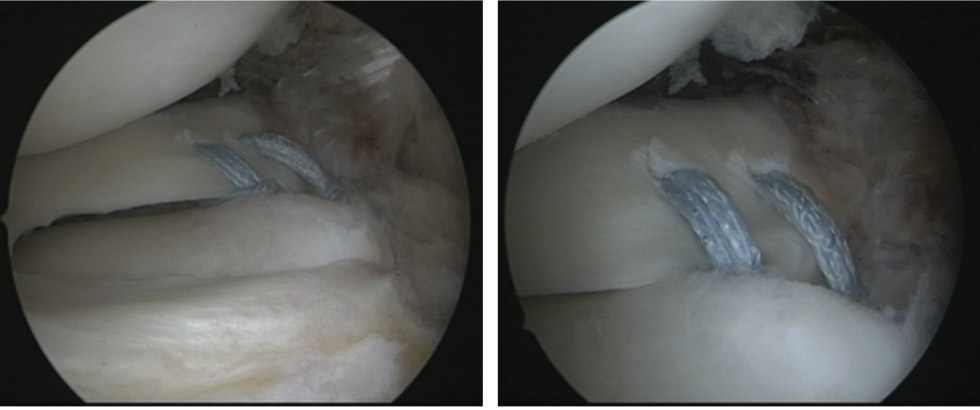
Figure 4: After transtibial pullout suture repair of lateral meniscus root with FiberTape.
Surgical Technique
An anatomic transtibial single-tunnel pull-out meniscalroot repair was performed using LaPrade et al. 12 technique.The patient was positioned supine with the surgical leg in 70°of knee flexion, the thigh secured in a leg holder. Standardmedial and lateral parapatellar arthroscopic portals were created.The posterior medial and lateral meniscus rootattachments were identified, and a calibrated arthroscopicprobe was used to assess root stability and, in the event that atear was identified, to characterize the root tear type. With acurved curette, the tibial attachment site of the torn meniscusroot was debrided of soft tissues down to a bleeding bone bedto improve healing of the repair. A 3-cm incision was createdadjacent to the tibial tubercle on the ipsilateral side of the roottear. One transtibial tunnel was drilled 5 mm apart, exitingintra-articularly at the posterior root attachment site. Anaiming device with a cannulated sleeve was used to positiona drill pin. The tunnels were visualized arthroscopically toverify appropriate tunnel positioning and the drill pins wereremoved. The knee scorpion suture passer was used to passthe 2-0 Fiberwire suture at the posterior root of the lateralmeniscus. The 2-mm FiberTape suture was changed to 2-0FiberWire by reroute technique, which was then shuttled downthe posterior transtibial tunnel (Figure 4). The steps wererepeated with a second suture passed through the midportionof the torn meniscus root and shuttled down the sametranstibial tunnel. The sutures were tensioned to reduce themeniscus root to its native anatomic attachment site. Ananatomic repair was performed because nonanatomic rootrepair fails to restore the contact area and mean contactpressures to those of the intact knee or those achieved withanatomic repair. Once the reduction of the root repair wasverified under direct arthroscopic visualization, the sutureswere tied over a surgical cortical fixation device on theanterior tibia.
Rehabilitation
Patient remained non-weightbearing in a straight leg bracefor the first 6 weeks after surgery to prevent isolated hamstringactivation, which could impart stress on the meniscal rootrepair. Partial weightbearing began at week 7 and graduallyincreased to full weightbearing as tolerated without pain orswelling. Patient focused on endurance and strength exercisesstarting at 2 months postoperatively and gradually progressedto normal activities with an average return to full activities at5 to 7 months postoperatively.12
Despite improving the identification of other meniscus tearpatterns on MRI, a high percentage of LMPRT is still missed.From our case the MRI showed normal morphology and signalintensity of both menisci but after arthroscopic probe, weidentified a completely torn lateral meniscus root from tibiainsertion.
Posterior lateral meniscus root tears (PLMRTs) areusually traumatic in nature and have been reported in 7-12%of patients with a tear of ACL.13
The surgeon should maintain a high level of suspicion andprepare the patient and operation for posterior lateral meniscusroot repair especially in cases of anterior cruciate ligamentreconstruction surgery due to the probability of highconcomitant injury. Finally, the posterior root of the lateralmeniscus should be carefully probed at the time ofarthroscopy, especially in cases of ACL injury.