The American Spinal Injury Association (ASIA) Impairment Scale (AIS) is a tool for grading the severity of spinal cord injuries.1 Although a number of studies have questioned the reliability and validity of this scoring system, it remains the gold standard tool for spinal cord injury evaluation.1-3 Under this system, motor function is assessed by 10 key muscles while sensory function is assessed by pin-prick and fine touch sensation with classification as grade A (complete spinal cord injury) to grade E (normal spinal cord).4 Although a direct association between AIS and neurological outcome has been observed,5 sensory function consists of mechanoreceptor, proprioceptor, temperature receptor and nociceptor modalities. Omission of any one of these modalities could affect the reliability of the AIS scoring system.6-9 While fine touch and proprioceptive sensation are located in the same pathway, dissociation between these two modalities has been reported.10,11 which suggests the need for assessment of multiple sensory modalities in spinal cord injuries, not just pin-prink and find touch sensation.
In 2013, a healthy 33 year-old Thai male presented at a rural hospital emergency department with quadriplegia following a motor vehicle collision accident. He reported neck pain as well loss of sensation and movement below the elbow including both hands and in both lower extremities. Physical examination confirmed complete paralysis and anesthesia below C6 level. Deep anal pressure was negative with no voluntary anal contraction. The patient was diagnosed with grade A impairment and complete spinal cord injury, according to the ASIA assessment protocol. Since there was no orthopedist or neurosurgeon available at the initial hospital, he was transferred to a provincial hospital under Gardner – Well tong immobilization twenty-four hours after the injury. At the provincial hospital, the service orthopedist recognized the preservation of joint position sensation and suspected an incomplete spinal cord injury. Cervical spine computed tomography revealed a bilateral facet fracture dislocation with 100% displacement and canal compromise at the C6 – C7 level (Figure 1). Magnetic resonance imaging was not performed due to unavailability of equipment.
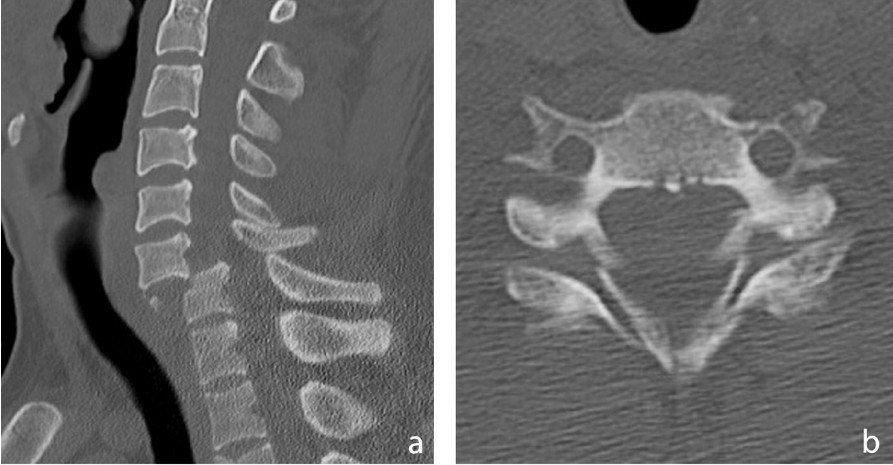
Figure 1: Cervical spine computed tomography revealed a bilateral facet fracture dislocation with 100% displacement and canal compromise at the C6-C7 level.
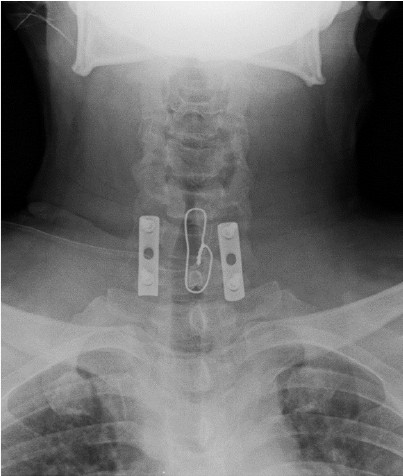
Figure 2 : A 1/3 tubular plate was applied using lateral mass 3.5mm screw fixation augmented by spinous process wiring.

Figure 3: Patient was able to walk assisted by cane around his residence and perform basic activities of daily living.
Diagnosis
Bilateral facet fracture dislocation of C6-C7 associated with incomplete spinal cord injury was considered the most likely diagnosis. However, according to ASIA/ISNSCI grading, this patient could be classified as AIS grade A – complete spinal cord injury.
Treatment
The patient underwent a successful emergent posterior open reduction and instrumentation with posterior fusion twenty-six hours after the injury. A 1/3 tubular plate was applied using lateral mass 3.5mm screw fixation augmented by spinous process wiring (Figure 2). No immediate complications were observed.
Follow-up and outcome
The patient was discharged and transferred back to the hospital corresponding to his healthcare districts for rehabilitation two days after surgery after which he failed to follow-up. Five years later, the same patient appeared again at the same provincial hospital where he exhibited significantneurological improvement including 4/5 motor function in all four extremities. His hand function was markedly improved. His sensation was still decreased at the terminal of the limb. He was able to walk assisted by a cane around his residence and could perform basic daily life activities such as bathing, eating and dressing (Figure 3). He could perform instrumental and advanced activities of daily living such as programming with his personal computer and return to work as a programmer. He complained of some residual spastic tone in his left leg and difficulty in controlling bowel and bladder function. Plain radiographs showed a well-fixed posterior instrument with evidence of fusion and good alignment of the cervical spine (Figure 4).
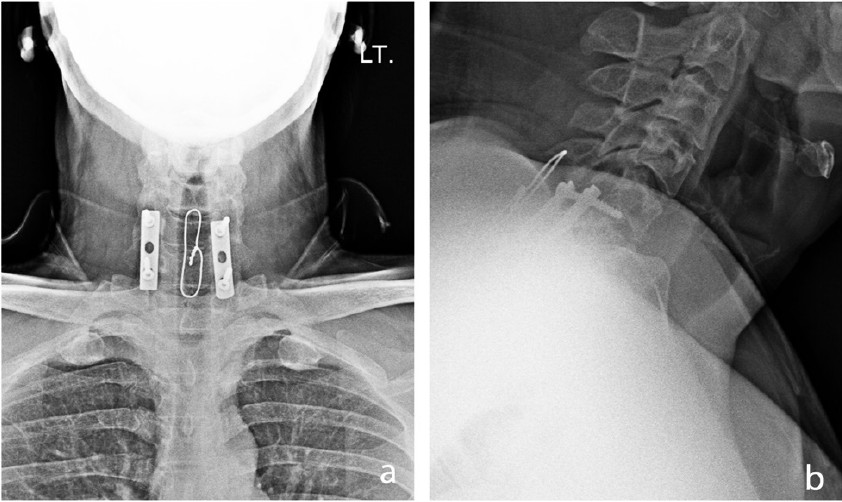
Figure 4: Plain radiographs showed a well-fixed posterior instrument with evidence of fusion and good alignment of the cervical spine
International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), published in 1982 by the American Spinal Injury Association (ASIA),12 helps identify motor and sensory grading in spinal cord injuries using the ASIA Impairment Scale (AIS) which is considered the gold standard for evaluating spinal cord injuries.1 This classification system is based on measurement of sensory and motor modalities. Sensory modalities are assessed by pin-prick sensation for spinothalamic tract and by light touch for posterior column of spinal cord according to the dermatome map. Motor function of 10 key muscles related to specific spinal cord segments are tested. Finally, the level of spinal cord injury is estimated according to the AIS scale which goes from A (complete injury) to E (normal).4 Using this classification system, a prognosis for neurological recovery and ambulation can be predicted. A patient with complete spinal cord injury (ASIA grade A) has the lowest chance of being able to walk independently after 1 year, while an incomplete injury (ASIA grade B to D) have a higher chance for recovery.5
The sensitivity, reliability and validity of the AIS scoring system had been questioned in several studies.2,3 One concern is that the sensory modalities testing relies only on pin-prick and fine touch, while there are actually four major sensory modalities: mechanoreceptor, proprioceptor, temperature receptor and nociceptor.6 Omission of one or more of these modalities could affect the reliability and validity of the scoring system.7-9
In the present case, the patient was diagnosed with a complete spinal cord injury according to the ASIA/ISNCSCI system even though there was preservation of joint position sense. Thus, it might have been more accurate to have diagnosed this patient with an incomplete spinal cord injury based on the preservation of at least one sensory modality. Preservation of a single sensory modality is not a common situation since both fine touch and proprioceptive sensation are located in the same pathway, the dorsal column – medial lemniscus (DCML) pathway.10, 11 However, the dissociation between these sensation modalities has been reported.11
The DCML pathway is located in the dorsal aspect of the spinal cord and travels into the brainstem and connects to the medial lemniscus. This pathway is responsible for fine touch, two-point discrimination, proprioceptive sensation and vibration sensation throughout the body with the exception of the head. In the ASIA/ISNCSI system, fine touch sensation is used as a proxy for all sensory modalities in the DCML pathway.
On the contrary to the ASIA/ISNCSCI grade prediction, the neurological outcome in the patient was very good after five years. A typical ASIA grade A is associated with only an 8.3% probability of independently walking at 1 year after injury.5 The outcome with this patient raises questions about the reliability of the ASIA/ISNCSI scoring system’s reliance on only two of four sensory modalities. Time to surgery is another factor which affects the recovery. Early surgery in traumatic spinal cord injury is significantly associated with better neurological outcomes.13 Interestingly, surgery was perferably performed less urgently in patients with ASIA grade A than in ASIA grade B to D patients.14
The use of other sensory modalities in assessing the severity of spinal cord injuries is recommended. Doing so can potentially improve the reliability and validity of the AIS scoring system, increase the accuracy of prognosis and potentially result in more favorable surgical outcomes.
I would like to express my thanks to Dr Lamar Robert for English language editing and review.