Cervicogenic headache is characterized by a chronic unilateral headache that radiates from the upper cervical spine. The trigeminocervical nucleus is a region of the upper cervical spinal cord where sensory nerve fibers in the descending tract of the trigeminal nerve (trigeminal nucleus caudalis) are believed to interact with sensory fibers from the upper cervical roots. This function convergence of upper cervical and trigeminal sensory pathways allows the bidirectional referral of painful sensations between the neck and trigeminal sensory receptive fields of the face and head.
Cervicogenic headache is pain radiated to the head from a source of the cervical spine. The terminology of cervicogenic headache and diagnostic criteria were proposed by Sjaastad in 1983.1 In 2004, The International Headache Society recognised cervicogenic headache as a distinct disorder,2 and a chapter in a headache textbook acknowledges that injuries to upper cervical joints can cause headache after whiplash.3
The prevalence of cervicogenic headache in clinical diagnosis is estimated to be 1%, 2.5% 4 or 4.1% 5 in general patients and as high as 17.5% among patients with severe headache.4 The prevalence is 53% in whiplash patients.6 The C2-3 zygapaphyseal joint involvement is the most frequent source of cervicogenic headache.8 The pathology of the atlanto-axial joint is probably the second most common source of cervicogenic headache but the true frequency is unknown.
The mechanism of pain has been widely debated8-10 but the pain probably stems from one or more structures of the neck.11 The trigeminocervical complex is a functional region of the upper cervical spinal cord where sensory fibers in the descending tract of the trigeminal nucleus caudalis are connected with sensory fibers from the upper cervical nerve roots. This functional convergence of trigeminal sensory pathways and upper cervical nerves allows the bidirectional referral of painful sensations between the neck and trigeminal sensory responsive fields of the face and head11 (Figure 1).
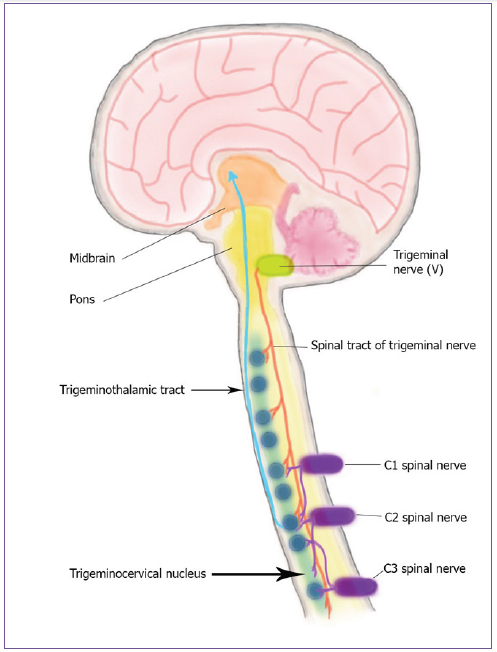
Figure 1: Pathophysiology of pain referral from the cervical spine to the head.
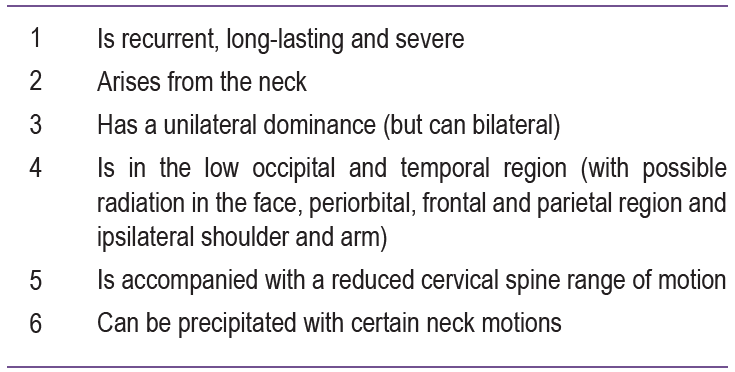
characterized as recurrent, long lasting, severe unilateral headache arising from the neck. The headache is usually affected on a unilateral side, but might also have presented on the contralateral side to a lesser degree. The affected side does not alternate from one side to the other (side locked unilaterally). The typical headache location is in the lower part of the occipital and temporal region and can radiate to periorbital area. The cervical spine usually has a reduced range of motion, and the headaches can often be precipitated by the patient with certain neck motions. Chou and Lenrow13 described criteria to include Cervicogenic headache (Table 1).
Table 1: The screening process of the systematic literature search.8
In a cervicogenic headache, there are various nerves that supply the cervical spine. The C1 spine nerve (suboccipital nerve) innervates the atlanto-occipital joint (C0-1). The pathology or injury affecting this joint is a potential source for pain that is referred to occipital region of the head. The C2 spinal nerve is in close proximity to the lateral capsule of the atlantoaxial (C1-2) joint and innervates the atlantoaxial and C2-3 zygapophysial joints; therefore, the pain is radiated from the occipital to parietal, temporal, frontal, and periorbital area. Ipsilateral eye lacrimation and conjunctival injection are common related signs. Arterial or venous compression of the C2 spinal nerve or its dorsal root ganglion has been suggested as a cause for C2 neuralgia in some cases.14-17
The third occipital nerve (dorsal ramus C3) is close to the C2-3 zygapophysial joint. This joint is prone to injury from acceleration deceleration (“whiplash injury”).18 Pain from the C2-3 facet joint is radiated either to the occipital or frontotemporal area.19
In referred pain, patterns have emerged with a painful stimulation of the cervical spine. The occipital pain was referred from posterior cervical muscles in early studies.20,21 Subsequent studies have shown the pain were produced from the stimulation of the atlantooccipital and atlantoaxial joints22, the C2-3 zygapophysial joint,23 the upper intervertebral disc and perhaps as far caudally as the C3-4 zygapophysial joint.24-26 (Figure 2).
In the terminology of occipital neuralgia, there is a specific pain disorder characterized by pain referred to sensory distribution of the greater or lesser occipital nerves,27 and the manifestation of occipital neuralgia are either a constant deep pain or burning sensation (Figure 3). The clinical pain presents as intermittent shooting or electrical-shock like. Paresthesia and numbness over the occipital scalp are usually present. There is difficulty in determining the definitive course of pain but greater occipital neuralgia is an outmoded diagnosis. There is no evidence of a pathology of the greater occipital nerve and this has not been proven to describe occipital pain. The proposal which the greater occipital nerve could be compressed between the posterior arch of the atlas and the lamina of the axis is incompatible with the anatomy and biomechanics of those vertebrae and was withdrawn by one of the authors who originally proposed it.28 Compression of the greater occipital nerve which takes off from the posterior neck muscles has not been discriminated from the normal anatomy of the nerve.29,30 Emancipation of the nerve has also not proved to be an effective measure.29,31 Deep aching pain is a tendency to be referred pain from an upper cervical joint.2,29
The cervicogenic headache is usually difficult to differentiate from a migraine. Neck pain and muscle spasm are common problems of a migraine attack.32-34 In a study of 50 patients with migraine, 64% complained of neck pain during a migraine attack, 31% producing neck pain in the prodrome period; 93%, during the headache phase; and 31%, during the recovery phase.32 Seven patients showed referred pain to the ipsilateral shoulder in the study by Blau and MacGregor.32
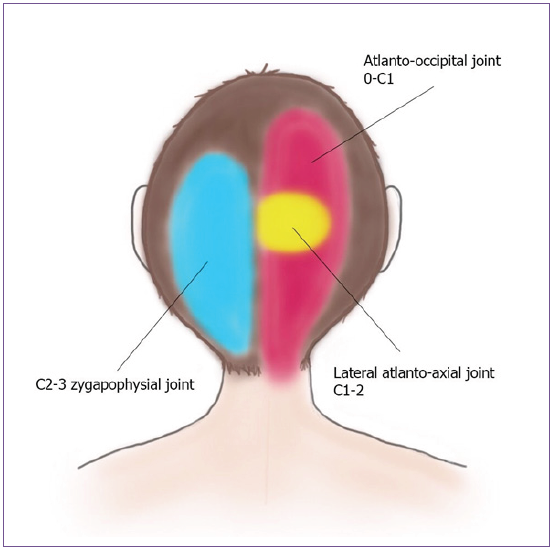
Figure 2: Referral pattern of upper cervical facet joint pain.

Figure 3: Sensory distribution of greater and lesser occipital erve.
The diagnosis of cervicogenic headache can often be made by clinical features as shown in Table 135 and first published in 1990 and revised in 1998.36,37 Results from subsequent studies have shown that these clinical diagnosis were either not specific to cervicogenic headache38-40 or were insufficiently distinct from healthy individuals.41,42
Diagnostic imaging such as radiography, magnetic resonance imaging (MRI), and computed tomography (CT) myelography cannot confirm the diagnosis of cervicogenic headache but can lend support to its diagnosis.43
The specific diagnosis of cervicogenic headache are diagnostic anesthetic blockade of the lateral atlanto-axial intraarticular joint, the C2-3 zygapophysial joint or the third occipital nerve and the C3-4 zygapophysial joint or the medial branches of the C3 and C4 dorsal rami, which supply the zygapophysial joint (Figure 4). The first three cervical facet joints that can refer pain to the head and Sjaastad’s criteria have been published, emphasizing the use of diagnostic nerve blocks in patients with cervicogenic headache as important confirmatory evidence.44
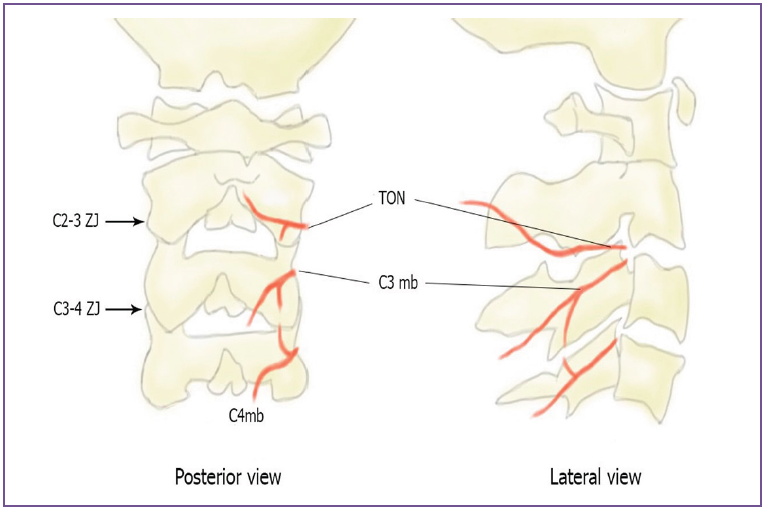
Figure 4: Showing median branch which supply facet joint. C3 mb = C3 medial branch, TON = third occipital, C4 mb = C4 medial branch, ZJ = zygapophysial joint.
Medication alone is not effective for this condition. Physical therapy with exercise is the preferred initial treatment because it is noninvasive and may provide long term improvement. The diagnostic procedures are medial branches injection or cervical zygapophysial intraarticular injection that can predict the outcome of radiofrequency neurotomy.45
In headache patients in whom there is a positive diagnostic injection at C2-3 zygapophysial joint (Figure 5) or medial branch (Figure 6) which supplies the C2-3 zygapophysial joint, the percutaneous radiofrequency neurotomy at third occipital nerve and C3 median branch (Figure 7) is proposed for long term relief of pain. This procedure includes the application of a radiofrequency needle parallel and close to the nerve where it crosses the joint, and using heat lesioning to disrupt the offending nerve.46 The study showed complete relief of pain was achieved in 88% of patients47,48 with a median duration of relief of 297 days.47 For recurrence pain, a repeating radiofrequency neurotomy should be done. The study reported that some patients had been able to maintain headache relief for longer than 2 years.47 The results of a randomized, placebo-controlled study indicate that responses to radiofrequency neurotomy are not due to placebo effects (p = 0.03).48
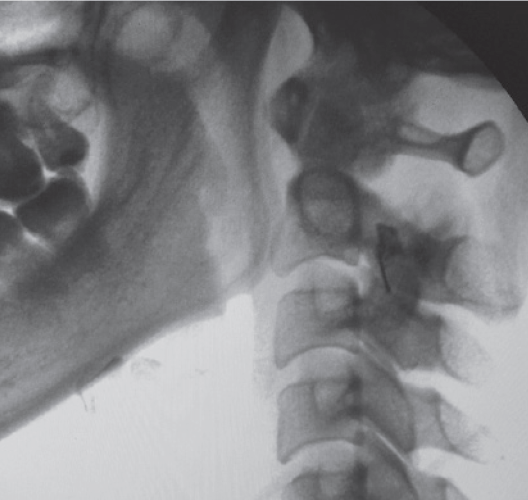
Figure 5: A lateral radiography demonstrating the needle placement for injection of C2-3 facet joint (Periarticular contrast spreading).

Figure 6: A lateral radiography demonstrating the needle placement for injection of C3 Medial branch.
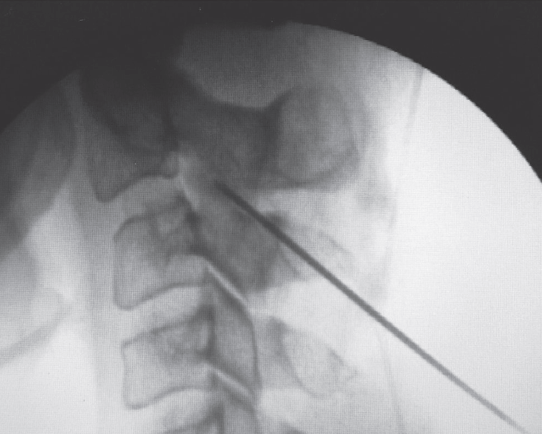
Figure 7: A lateral radiography demonstrating the Radiofrequency needle placements for ablation of third occipital nerve (TON).
Surgical procedures for cervicogenic headaches are not recommended unless there is compelling evidence of a surgically amenable lesion that is refractory to all reasonable nonsurgical treatment. Surgery may be beneficial for three specific causes of cervicogenic headache:49
Cervicogenic headache is a relatively common problem that is usually misdiagnosed or unrecognized. The clinical symptom can be similar to that of the more commonly encountered primary headache disorders such as migraine or tension-type headache. Early diagnosis and treatment by a multidisciplinary team including especially a neurologist and pain specialist can significantly decrease disability and can increase quality of life.
