In the standard care of trauma patients, established by the ATLS course, physical examination is always done with the patient in a supine position.1 Occasionally, this position may not be practical for patients who present with an injury in less common site(s), affecting the assessment and monitoring process, which in turn could lead to limitations in decision making and inappropriate management of the injuries.
A 53-year-old Malaysian female patient presented at the hospital’s emergency (ER) department (as a walk-in) arriving via public motorcycle service after being assaulted by a known assailant 30 minutes prior to arrival at the hospital.
Patient arrived at ER, escorted by her employee. The employee reported that the patient had been assaulted by her ex-employee. The assailant stabbed her in the abdomen around the epigastrium and attempted to slit her throat. He delivered his final attack by stabbing her in the back, leaving the knife in the left side of her mid-back.
On the primary survey, physical exam was completed while the patient assumed right decubitus position due to the retained knife on her back (Figure 1).
Upon initial examination, her airway was intact with normal voicing. Her breathing showed mild dyspnea although both lungs remained clear with equal breath sounds bilaterally on auscultation. Oxygen saturation was detected at 85% on room air. Her blood pressure was measured at about 98/65 mmHg while pulse rate (PR) was at 85 beats per min (bpm) on arrival. Variations in blood pressure were between 80/40-118/87 mmHg; while her PR was between 48-101 bpm during the resuscitation process in the resuscitation room. Her Glasgow Coma Scale (GCS) was 15 (E4V5M6) at time of arrival. The neck region showed multiple wounds on the neck, in which, multiple lacerated wounds were observed on the left side of her neck deep to the dermis layer (Figure 2). Wounds were also detected in other regions of the body including the epigastrium and back. The wound on the epigastrium measured about 4-5 cm. A vertical lacerated wound was observed on the epigastrium without active bleeding (Figure 3). The retained knife on her left thoracic back was observed without active bleeding around the penetrating site (Figure 1).

Initial management in the emergency department was immediately implemented. Upon completion of physical examination, we performed tube-thoracostomy on her left chest; however, there were no bodily fluids or content obtained post insertion on right decubitus position. Management of patient’s hemodynamic status was done by intravenous (IV) resuscitation, in which we chose Ringer lactate solution on maintenance rate via 2 IV catheters for the patient. Focused Assessment with Sonography in Trauma (FAST) was performed with a negative finding while the patient resumed right lateral decubitus position. Portable chest x-ray was also performed in a right lateral decubitus position (Figure 4). Insertion of nasogastric tubes (NG-tube) was completed with no blood content observed. Urinary in-dwelling catheter was inserted and retained.
After initial management, an operation was the selected choice of treatment due to variations in vital signs with a period of hemodynamic instability. Left anterolateral thoracotomy was initially performed on right lateral decubitus position (Figure 4) because the finding from the chest x-ray revealed that the retained knife was close to the thoracic aorta. Per thoracotomy findings, there were no penetrating injuries on any intra-thoracic organs and the pleural layer was intact. With the finding above, we proceeded with closing the thoracotomy site and removed the knife (Figure 5). The wound on the back was closed with a Penrose drain and retained.
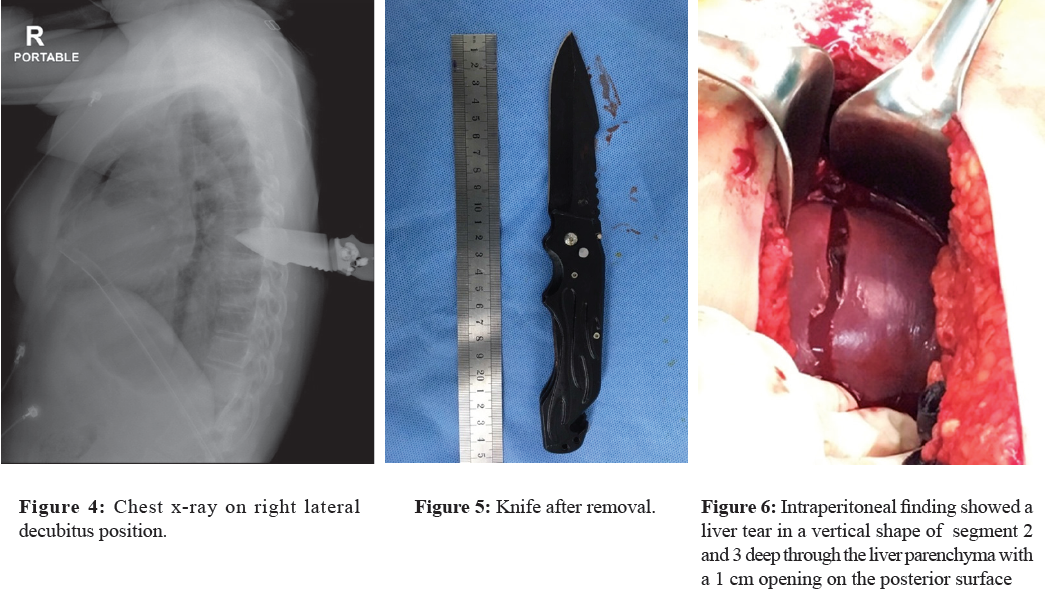
Thereafter, we performed an explore-laparotomy on the upper midline with liver segment 2 and 3 showing a vertical laceration of about 5 cm length, cut deep through liver parenchyma with a 1 cm wide opening on the posterior surface (Figure 6). Hemoperitoneum was observed and measured about 900 ml. Otherwise, internal organs especially the diaphragm, stomach and suprarenal aorta remained intact with normal appearance and no injury detected.
The liver was repaired by Catgut 1-0 with Surgicel® original mesh packing on anterior wound surface. Catgut 1-0 simple suture was used to repair the posterior surface of liver. Peritoneal lavage was done with round Jackson-Pratt drain inserted and retained on subhepatic region. Abdominal wall was closed in layers.
Post-operatively, patient had an atrial fibrillation ranging between 140-150 bpm and a right pleural effusion on day 2 after operation, which was adequately controlled by intravenous amiodarone and volume restriction regimen for balanced fluids respectively. On day 4 post-operatively, extubating was completed with success. Oral diet and ambulation activity were introduced to the patient. All drainage catheters were removed on day 5 post-operatively. On day 7 post-operatively, rebleeding occurred from dorsal branch of left posterior intercostal artery on the wound at the back after removal of Penrose drain. The re-bleed was managed and controlled by ligation, and wound closure was completed with smaller Penrose drain retained again in the operating room.
All stitches were removed, and the patient was discharged on day 10 post-operatively. An appointment was made for the patient for a follow up visit to re-evaluate the wound. Penrose drain was removed from the wound on the back on day 4 after the patient was discharged from the hospital. The final visit for the patient was on day 8 after being discharged from the hospital.
A 53-year-old female who was stabbed by a knife on the epigastrium and left posterior chest presented at emergency department on right lateral decubitus position due to a retained knife on the back. Standard ATLS approach was performed with limitations in this case and complete investigations, especially CT-whole body were not possible due to the variance of the patient’s vital signs. Since an aortic injury could result in a fatal condition prior to the removal of the knife, we had to ensure that there was no extensive and major injury, in which the knife injured or stabbed the thoracic aorta.2-4
Given the position the patient assumed, a proper physical examination was not possible to complete. Patient’s vital signs showed variance. Aortic injury from the stabbed wound on the back and cardiac tamponade due to the trajectory of the stabbed epigastrium which is often superoposterior made it impossible to rule out an injury to the diaphragm and pericardium. In a right decubitus position, FAST cannot be reliable.5,6 Left tube-thoracostomy was done initially and left thoracotomy was performed immediately in order to rule out thoracic aorta and pericardium injury before removal of the knife. In this patient, left thoracotomy was performed, in which, no injury to the pleural cavity was found.7 With this finding, removal of the knife was considered safe and appropriate. Retained knife was removed, and then the stabbed wound on the back was closed accordingly.
As for the stabbed wound on the epigastrium, we thought that there could be an intraperitoneal organ injury; therefore, an exploration laparotomy was performed to investigate and detect any possible injured organs and these were repaired accordingly.8-10 On laparotomy, there was 900ml. of hemoperitoneum, and a liver injury was found on anterior surface of segment 2 and 3 in a vertical shape with the opening through the posterior liver surface.11 Liver irrigation with simple closure with Surgicel® buttress was done on both surfaces of the liver.12 The amount of blood shown in the peritoneum (approximately 900 ml.) combined with the blood loss at the scene was sufficient evidence to explain the rationale of presentation of shock in the emergency department.
However, due to the hemodynamic instability of the patient and the risk factors, the surgical team was obliged to take a quick decision and to act immediately in order to ensure the safety of the patient.
When trauma patients present at the ER in an unusual position this can lead to limitations in the physical examination, monitoring and imaging investigations as errors can affect the analysis of the findings and the treatment delivered, and this in turn can lead to inappropriate or over management. However, surgeons must always consider patient’s safety as the first priority and carefully take in all the possibilities to ensure that life-saving measures have been efficiently delivered to the patient.