Chronic lumbosacralradicular pain (CLRP) is a common problem in the pain center. Options of treatments are medication, physiotherapy, epidural steroid injection and surgery when conservative treatment fails.
Epidural steroid injection (ESI) is the most common intervention in pain centers.1 Moreover, there are various techniques of epidural steroid injection but transforaminal technique was preferred to interlaminar approach or caudal epidural steroid injection1,2 because with this approach, the needle tip is close to the nerve root, not requiring large injected volumes to the pathologic site.3 There were two techniques in the transforaminal approach. The infrapedicle transforaminal approach in which the needle tip is advanced into “safe triangle” below the pedicle4,5 and the retrodiscal transforaminal approach in which the needle tip is on the suprapedicle level and posterior to the disc.3
That said, the S1 nerve root approach is unique as there is a sacral nerve root travelling out from the S1 foramen of sacrum. Therefore, the S1 transforaminal technique, in which we can perform an injection via the S1 foramen would be preferable to the retrodiscal technique.
Since the efficacy of each technique in S1 radicular pain management was relatively unknown, the objective of this present study was to determine the efficacy of the L5-S1 retrodiscal technique and the S1 transforaminal technique in L5-S1 spinal stenosis with S1 radicular pain
Once the Institutional Review Board of Royal Thai Army Medical Ethics Committee’s approval was received, at Phramongkutklao Hospital from September 2014 to September 2015, all participants provided informed consent. Forty adults, aged 18-80 years, who had a history of chronic S1 radicular pain (longer than 6 months), unsatisfactory pain control with oral medication, physiotherapy or previous epidural steroid injection and no indication for surgery were enrolled in this study. Those patients who had significant neurological deficits or cauda equine syndrome, coagulopathy, history of allergy to local anesthetics, contrast media, triamcinolone, psychiatric problem, pregnancy and language barrier were excluded.
The participants were interviewed and examined by pain physicians. All neurological signs and symptoms were documented. They were randomly allocated into two groups equally; the retrodiscal group (R-group) received a L5-S1 retrodiscal epidural steroid injection, and the S1 transforaminal group (S-group) received a S1 transforaminal epidural steroid injection. A computer-generated table was used to allocate participants. All of the participants and the outcome assessor (trained nurse) were blinded to the study group.
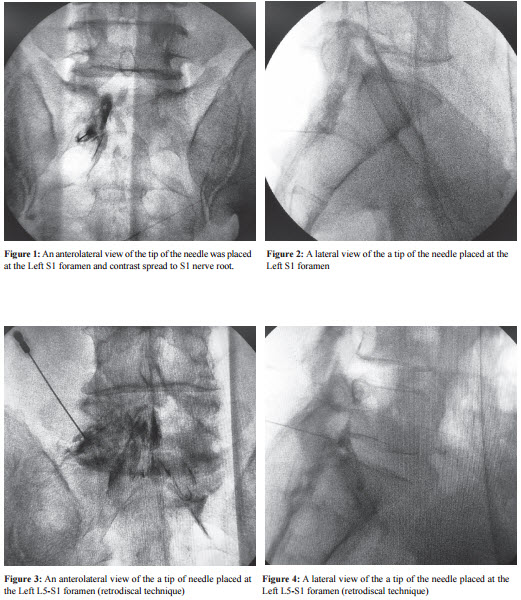
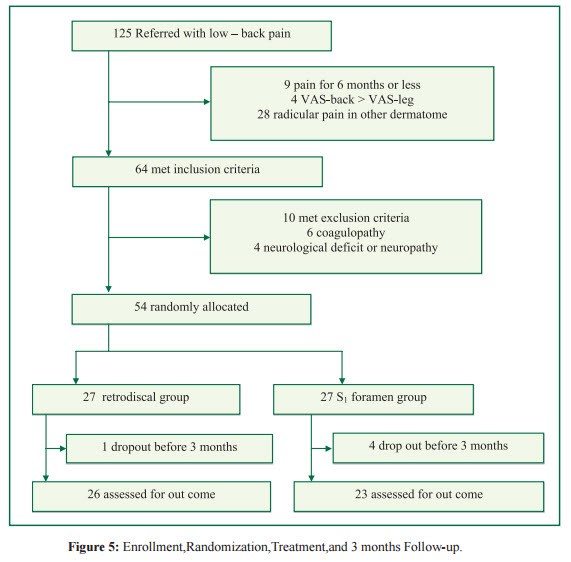
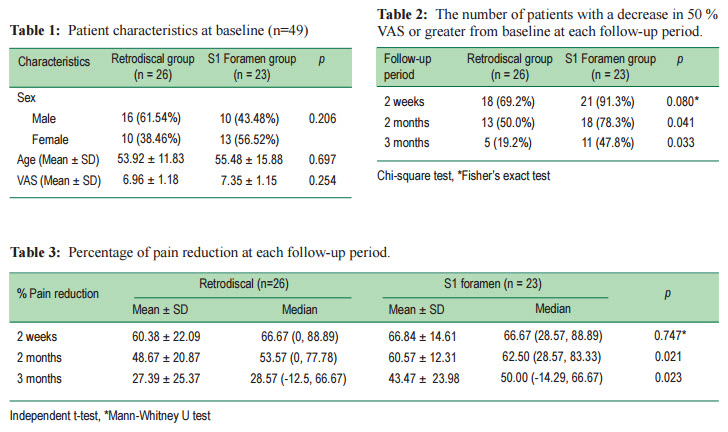
The intervention was performed as an outpatient procedure using local anesthesia and intravenous sedation when necessary. With the patient in the prone position, pulse oximetry and automated blood pressure monitoring were used. The lower back and buttock areas were cleaned and prepared under sterile technique. The C-arm image intensifier (BV Pulsera, Philips®, Netherlands) was positioned into oblique view 20-25 degree ipsilateral to the painful side in R-group and into the AP view in S-group.Afterskin infiltration a 22-G, 10 cm long, Quincke spinal needle (Spinocan®, B.Braun MelsungenAG, Germany) was inserted in the direction of the radiation beam. When the tip of the needle was located in the middle on the intervertebral foramen in lateral view, non-ionic contrast media (Iopamiro 300, Bracco s.p.a.®. Italy) was injected to confirm a needle location in both the S-group (Figure 1,2) and R-group (Figure 3,4). Both groups were injected with 2 ml of 0.125% bupivacaine (Astra Zeneca, Sweden) plus triamcinolone 40 mg(L.B.S.Laboratory Ltd., Bangkok, Thailand).
All participants were evaluated by a blinded assessor before treatment, at the 2 week, 2 and 3 month periods after the procedure was performed using VAS (visual analog scales;0-10 scale).The outcome was a comparison of the efficacy of procedure between groups. The effective response to the procedure was defined by as a 50 point-reduction of VAS from the baseline.6
Based the pilot study, the average percentage of VAS reduction from the baseline at 2 months are is 42.7 (SD = 23.4) in R group and 61.8 (SD = 16.7) in S group with a 90% power of test. The sample size calculated in each group was 24
However, this present study added 10% for to compensate for compensation the number of patients who did not come for follow up. The final number of patients in one group was 27. The outcome was analyzed by an intension-to-treat with the decision rule and all data were analyzed with the Statistical Package for Social Science (SPSS for Windows, version 15.0)
The categorical data was presented as a percentage. The continuous data was shown as either mean±SD in normal distribution data or median, max-min for non-normal distribution data.
The number of patients who had at least 50% VAS reduction from baseline was defined as responding to procedure that and this was presented as a percentage using the Chi-square test or Fisher’s exact test for a comparison between groups. Independent t-test or Mann-Whitney U test were used for comparing the percentage of VAS reduction between groups. Two-way repeated measure ANOVA was used to compare the VAS between groups over times and a p value of less than 0.05 was considered as statistically significant.
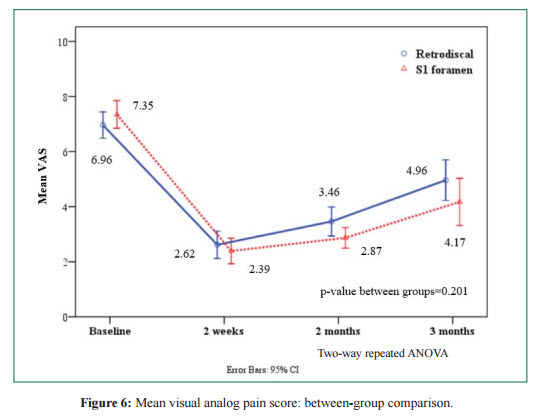
Of the 125 patients referred, 54 patients met the inclusion criteria and were enrolled, of whom 27 were randomly allocated to both the retrodiscal group (R-group) and the S1 foramen group (S-group). Five patients dropped out (one R-group, four S-group) because of a rapid deterioration of symptoms within 3 months after treatment. All five needed surgery because of progressive weakness caused by a herniated disc and spondylolithesis. These patients were not part of the follow-up group. (Figure 5).
From the 49 enrolled patients, there were a remaining 26 patients in the R-group and 23 patients in the S-group who could be assessed for outcome. There were no significant differences in the demographic data between the retrodiscal group (R-group) and the S1 foramen group (S-group) with respect to sex (p = 0.206), age (p = 0.697) and the pre- procedural pain intensity (p = 0.254) (Table 1). The VAS of both groups was reduced after receiving the procedure for 3 months. However, it gradually increased but did not get higher than the pre-procedural intensity in both groups. The S-group had a lower VAS compared to the R-groups but there was no statistically significant difference between groups over time with the two-way repeated ANOVA (p = 0.201; Figure 6).
The number of patients who responded to the procedure was isshown inTable 2.The S-group had amore significantresponse to the procedure in the 2 and 3-month follow-up (Table 3),(p = 0.041 and 0.033 respectively).Furthermore, neither adverse effects nor complications were reported
Transforamianal epidural steroid injections (TFESI) have been used to treat chronic lumbosacral radicular pain for decades. However, the effective response to TFESI is based on the basis of precise location of the needle tip and injected volume.7-9 Several previous studies investigated contrast spreading 7-10 Furman MB et al.8 mentioned that 100% ipsilateral spreading of contrast media in S1-TFESI with injection volume of 2 mL but 92% superior spreading to superior aspect of L5-S1 intervertebral disc after 3 mL of contrast and 27% beyond midline contrast spreading after 4 mL. The present study found that 2 mL injected volume in the S-group was spread along the S1 nerve root but the injected volume was more of a cephalad spread at the L5 nerve root than the S1 nerve in the R-group which was in accordance with the study of Kim C.7 and performed about 60% mostly spread over the proximal nerve root of the level of the procedure therefore there was a lower pain reduction in R-group. Moreover, the tip of the needle in the S-group was closer to the S1 nerve root than the R-group, therefore the S-group was more effective than the R-group.
This study has several limitations. Firstly, the study was based only on clinical symptomatology which can be misleading, so a diagnostic block should be done before including the patient however there is no practical treatment in the hospital studied. Secondly, psychological issues or functional outcome were not addressed in this study. Thirdly, this present study was a comparison only between the retrodiscal approach L5-S1 foramen and the S1 transforaminal approach. We did not compare these to the traditional approach (infrapedicle approach), therefore this present study did not investigate the effectiveness of the traditional injection at L5-S1 foramen for S1 radicular pain. However, in the case of the traditional (infrapedicle) approach, there are numerous cases where the injected drug would flow into the cephalic root of the nerve root.11 Fourthly, some patients have various diseases which means there might be confounding factors of the results. Fifthly, other treatment modalities were not controlled such as medication, physiotherapy, psychotherapy as well as the placebo effect.
This study showed S1 transforaminal technique provided an advantage over the L5-S1 retrodiscal technique in reducing S1 radicular pain at the 2 and 3-month period with no neurological deficit. Consequently, the use of this transforaminal epidural steroid injection at S1 foramen as routine treatment in S1 radicular pain should be advocated
The authors declare that there is no conflict of interests regarding the publication of this paper.
The authors would like to thank the patients who participated in the trial, the referring medical doctors, Miss Pimrapat Tengtrakulchareon for her statistical advice and data analysis. We also wish to thank the anesthetic and orthopedic staff for their cooperation. This research was approved by the Institutional Review Board of Royal Thai Army Medical Ethics Committee’s approval at Phramongkutklao Hospital (ref number S037h/57 Date: 20-December-2014).